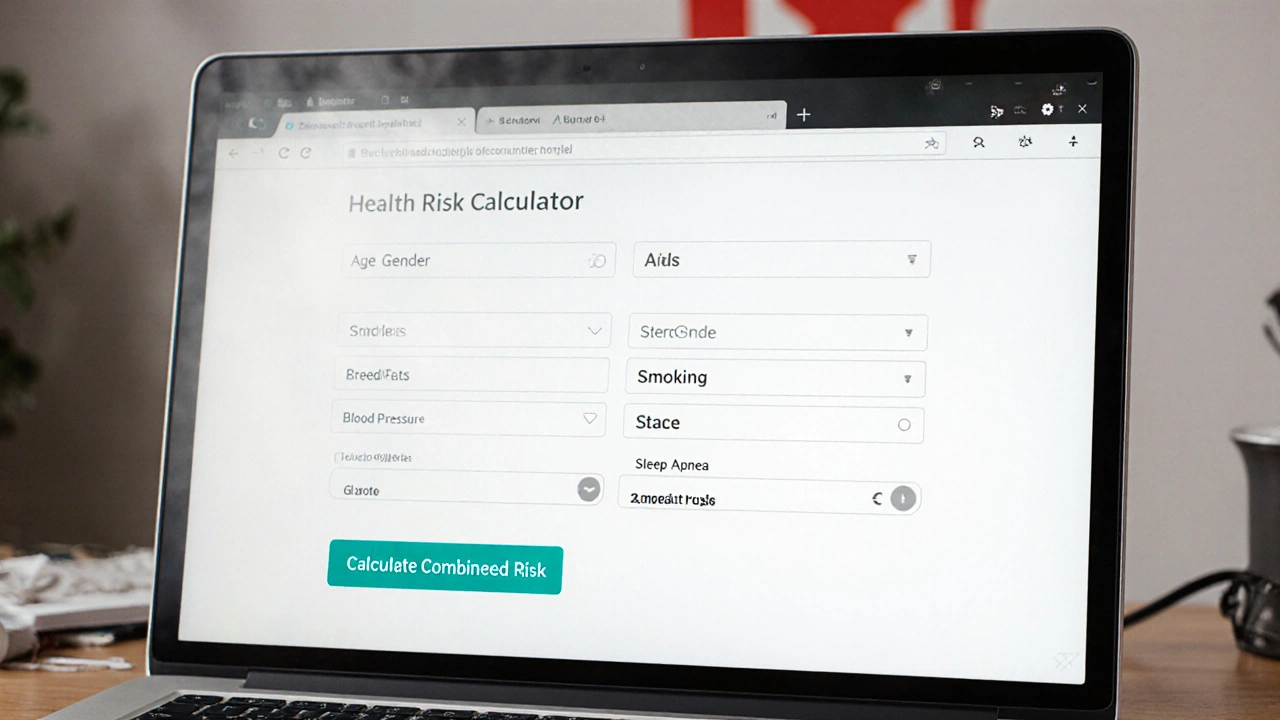
Enter your details and click "Calculate Combined Risk"
This tool estimates the relative risk of experiencing a TIA or stroke given shared risk factors with sleep apnea. It considers age, gender, BMI, blood pressure, smoking status, and sleep apnea history.
Note: This is a simplified estimation tool and does not replace clinical assessment. Consult a healthcare provider for personalized advice.
When blood flow to a part of the brain stops for a brief moment, the brain tissue experiences a short‑lived shortage of oxygen. This event is called a Transient Ischemic Attack (TIA). Symptoms-such as sudden weakness, slurred speech, or vision loss-usually resolve within 24hours, often within minutes.
Although the effects fade, a TIA is a red flag. Studies from 2023‑2024 show that up to 40% of people who have a TIA experience a stroke within the next five years if no preventive steps are taken.
Sleep apnea describes repeated pauses in breathing during sleep. The most common form, Obstructive Sleep Apnea (OSA), occurs when throat muscles collapse, blocking the airway. A night of OSA can involve 20‑30 interruptions, each lasting 10‑30seconds, jolting the brain out of deep sleep.
Typical signs include loud snoring, choking sensations, morning headaches, and excessive daytime sleepiness. In the United States, about 22% of adults have moderate‑to‑severe OSA, yet many go undiagnosed.
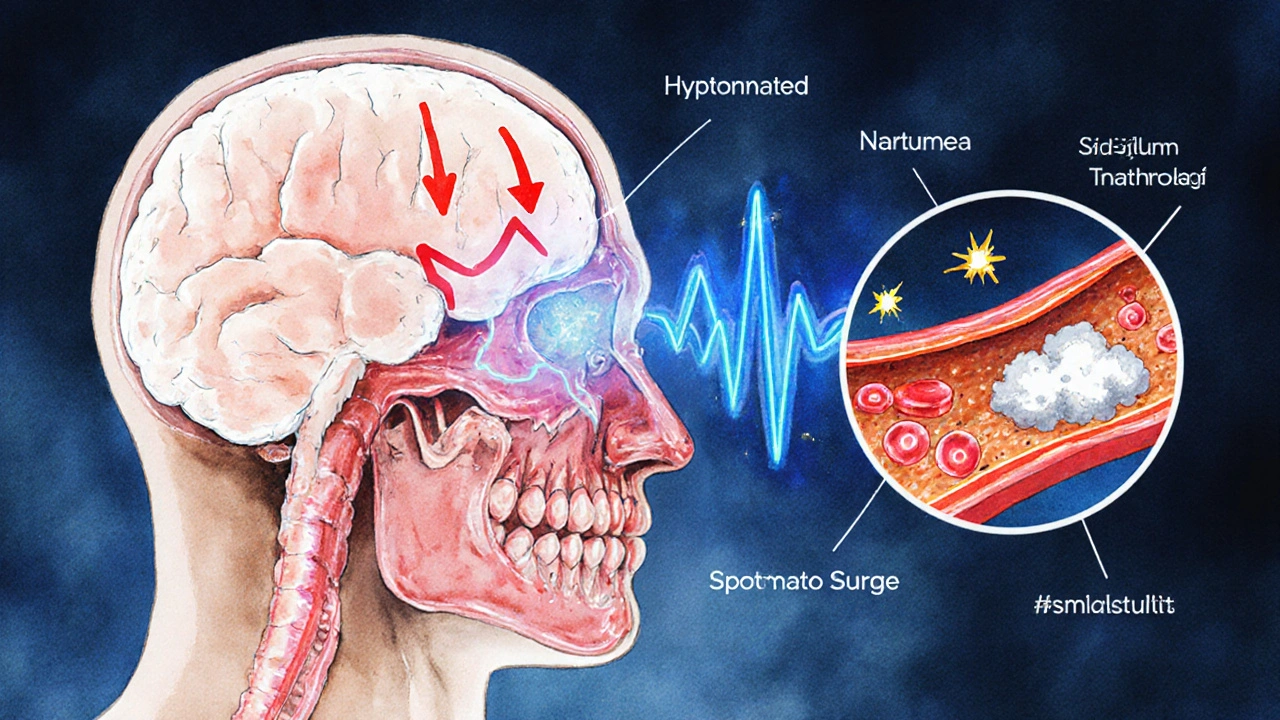
The link between TIA and sleep apnea is not a coincidence. Several physiological pathways converge:
When these mechanisms stack on top of classic TIA risk factors-high blood pressure, diabetes, smoking-the probability of a “mini‑stroke” rises sharply.
Both conditions thrive on a similar set of lifestyle and medical variables:
Addressing these factors improves outcomes for both ailments.
Stroke risk is magnified when OSA and TIA coexist. A meta‑analysis published in the Journal of Stroke & Cerebrovascular Diseases (2024) pooled eight cohort studies and found:
| Group | Annual Stroke Rate | Hazard Ratio (HR) |
|---|---|---|
| TIA+Untreated OSA | 3.2% | 2.1 |
| TIA+Treated OSA (CPAP) | 1.5% | 1.0 (reference) |
| TIA+No OSA | 1.4% | 0.9 |
The data show that effective OSA therapy can bring the stroke risk of a patient with both conditions down to the level of someone without sleep apnea.
Because many sleep‑apnea sufferers are unaware they have the condition, clinicians now recommend routine screening after a TIA. Typical steps include:
Early identification is key; the earlier CPAP (continuous positive airway pressure) therapy starts, the greater the protective effect.

Treatment plans should tackle the root causes and the symptoms.
Coordinated care between neurologists, sleep specialists, and primary physicians ensures that each aspect is monitored.
Even without a formal diagnosis, certain habits shrink the odds of both TIA and sleep apnea:
If you experience any of the following, call emergency services (000 in Australia) or head straight to the nearest hospital:
Even if symptoms fade quickly, a TIA is a warning. Prompt evaluation lets doctors start preventive therapy before a full‑blown stroke occurs.
Yes. Loud, chronic snoring, choking or gasping during the night, and observable pauses in breathing are common cues. Partners often report morning headaches in the person with apnea.
CPAP is the gold‑standard, but alternatives exist: oral appliances that advance the jaw, positional therapy (sleeping on the side), weight‑loss programs, and in severe cases, upper‑airway surgery.
Guidelines from the American Stroke Association (2024) recommend screening during the same hospital admission or within two weeks of discharge.
Clinical trials show an average 3‑5mmHg drop in systolic pressure after three months of consistent CPAP use, especially in patients with moderate‑to‑severe OSA.
Rarely, but possible. Rare clotting disorders or arterial dissection can cause a TIA even in otherwise healthy individuals. Nonetheless, checking for sleep apnea is still worthwhile because it often hides behind ‘no known risk’.
Jennifer Pavlik
5 10 25 / 15:31 PMIf you suspect sleep apnea, getting tested is a smart first step.
Jacob Miller
10 10 25 / 06:37 AMLooks like the calculator pretends to be helpful but really just throws numbers at you.
Anshul Gandhi
14 10 25 / 21:44 PMThe relationship between transient ischemic attacks and obstructive sleep apnea is far more than a coincidence.
Every epidemiological study that you skim over hides a hidden variable: the chronic intermittent hypoxia that the airway obstruction creates.
That hypoxia triggers systemic inflammation, endothelial dysfunction, and sympathetic over‑activity, all of which are classic precursors to atherosclerotic plaque instability.
When you add the fact that many patients with TIA have elevated circulating fibrinogen and C‑reactive protein, the puzzle pieces start to fit together like a jigsaw.
But the mainstream narrative conveniently omits the role of commercial CPAP manufacturers, whose lobbying power has shaped guidelines in subtle ways.
Are we seeing an over‑reliance on CPAP as a blanket solution because of a coordinated push from a few key industry players?
Moreover, the calculator’s linear weighting of risk factors betrays a simplistic view of a complex, non‑linear system.
For example, a BMI of 32 doesn’t just add two points; it multiplies the pro‑thrombotic effect of hypertension by a factor that current models ignore.
And smoking status-labelled as “current” or “former”-fails to capture the dose‑response curve that determines oxidative stress levels.
Let’s not forget the genetic predisposition to both OSA and cerebrovascular events, which is largely invisible in a web‑based form.
In short, while the calculator is a nice educational tool, it masks the deeper, possibly manipulated, realities of how we assess risk.
Take it with a grain of salt and always demand a full polysomnographic study before accepting any risk estimate.
Emily Wang
19 10 25 / 12:51 PMHey folks, just a quick reminder that lifestyle tweaks can make a huge difference.
Regular exercise helps lower blood pressure, improves sleep quality, and reduces the severity of apnea episodes.
Pair that with a balanced diet low in sodium and saturated fats, and you’re giving your brain a better chance to stay clear of those mini‑strokes.
Hayden Kuhtze
24 10 25 / 03:57 AMAh, another glorified spreadsheet masquerading as a medical marvel. Simple math, no real insight.
Craig Hoffman
28 10 25 / 18:04 PMQuick tip: use this tool as a conversation starter with your doc, not a diagnosis.
Samantha Leong
2 11 25 / 09:11 AMUnderstanding the link can feel overwhelming, but remember you’re not alone; many resources are available to guide you through the testing and treatment process.
Taylor Van Wie
7 11 25 / 00:17 AMThis is why we need a strong national health push-more funding for sleep labs and public awareness campaigns!
carlee Lee
11 11 25 / 15:24 PMSolid info-keep it concise, keep it clear.
chuck thomas
16 11 25 / 06:31 AMWhen we think about risk, we’re really pondering probability as a reflection of deeper systemic balance.
Sleep apnea tips that balance, and a TIA is a reminder that the system can wobble.
Gareth Pugh
20 11 25 / 21:37 PMImagine your arteries as a bustling highway; apnea throws traffic jams in the form of hypoxic spikes, and a TIA is the occasional fender‑bender that reminds you to keep the lanes clear.
Illiana Durbin
25 11 25 / 12:44 PMGreat points above-just to add, a thorough sleep study can reveal silent events that standard questionnaires miss.
Tyler Heafner
30 11 25 / 03:51 AMIt is advisable to consult a qualified physician for a comprehensive evaluation of both cerebrovascular risk and sleep‑disordered breathing.
ADam Hargrave
4 12 25 / 18:57 PMOh sure, just plug your details into a glorified calculator and expect a miracle. 🙄
Michael Daun
9 12 25 / 10:04 AMLove the idea but the form could use less jargon and more plain speak.
Rohit Poroli
14 12 25 / 01:11 AMFrom a clinical informatics perspective, integrating polysomnographic metrics with cerebrovascular risk algorithms could enhance predictive accuracy and streamline patient pathways.