
When a drug has a narrow therapeutic index, the difference between helping you and harming you is razor-thin. Theophylline is one of those drugs. Used for decades to treat asthma and COPD, it still saves lives today - but only if its levels in the blood are watched closely. Skip the monitoring, and you risk seizures, heart rhythm problems, or even death. Skip it, and you might not get any relief at all. There’s no middle ground.
Theophylline isn’t just any bronchodilator. It’s a methylxanthine that works by relaxing airway muscles and reducing lung inflammation. But its magic only happens in one narrow window: 10 to 20 mg/L. Go below 10, and it barely works. Go above 20, and your risk of serious side effects shoots up. Above 25? That’s a medical emergency. Seizures, irregular heartbeat, vomiting, confusion - these aren’t rare. They’re predictable.
Why does this happen? Because theophylline doesn’t behave like most medications. Its metabolism isn’t linear. A small increase in dose - say, from 300 mg to 400 mg - can cause your blood level to jump by 50% or more. That’s not normal. Most drugs increase slowly with dose. Theophylline? It can explode.
Doctors can’t guess the right dose. Even experienced ones can’t. Two people taking the same 400 mg tablet might have blood levels that differ by 100%. One might be perfectly safe at 14 mg/L. The other might already be at 28 mg/L - heading for the ER.
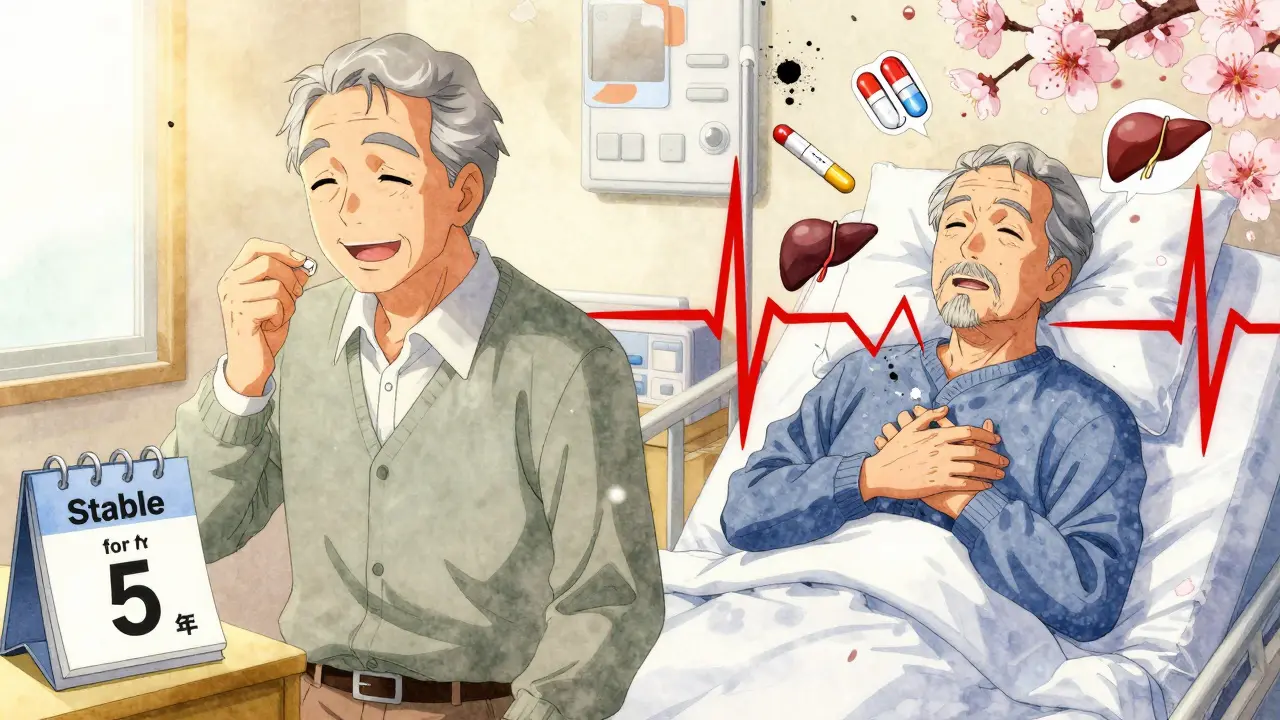
Why such wild variation? Because your body changes. Smoking? It speeds up theophylline breakdown by nearly 60%. Stop smoking? Your levels can spike overnight. Liver disease? It cuts clearance by half. Pregnancy? By the third trimester, your body clears it 40% faster. Age? After 60, liver function drops. That means older patients need lower doses - but they often get the same as younger people.
And then there are the drugs. Antibiotics like erythromycin or ciprofloxacin? They can double theophylline levels. Antifungals? Same. Even cimetidine (a common heartburn pill) can push levels into toxic territory. On the flip side, carbamazepine (for seizures) or St. John’s Wort (a herbal supplement) can slash levels so much that your asthma flares up. You don’t even know it’s happening.
You can’t just test once and forget it. Timing matters. For immediate-release theophylline, draw blood right before the next dose - that’s the trough. That’s when levels are lowest and most telling. For extended-release tablets? Wait 4 to 6 hours after taking it. Test too early, and you’ll overestimate. Test too late, and you’ll miss the peak.
Start monitoring 5 days after beginning treatment. Why? That’s how long it takes to reach steady state. After that, check every 6 to 12 months if you’re stable. But if you’re over 60? Every 3 to 6 months. Heart failure? Every 1 to 3 months. Pregnant? Monthly. Any new medication? Test immediately. Changed your smoking habit? Test. Had a big night out drinking? Test.
One 2023 case in Cureus showed a 68-year-old man with COPD who started ciprofloxacin for a urinary infection. Three days later, his theophylline level hit 28 mg/L. He went into ventricular tachycardia. He survived - barely. He’d never been monitored before. His doctor assumed the dose was fine because it had worked for years. It didn’t account for the new drug.
Don’t just look at the number. Watch the person. Are they jittery? Insomniac? Nauseous? Those are early signs. Heart rate over 100 beats per minute? That’s a red flag. Low potassium? Theophylline and asthma drugs like albuterol both push potassium out of cells. Low potassium makes arrhythmias more likely.
Check blood gases if breathing is labored. Look at liver enzymes. Check kidney function - theophylline is cleared by the kidneys too. A 2022 study in the Journal of Asthma found that hospitals with formal monitoring programs cut adverse events by 78%. Why? Because they didn’t just check levels. They checked everything: heart rate, breathing, electrolytes, meds, smoking status.
In the U.S., about 1,500 people end up in emergency rooms every year because of theophylline toxicity. About 10% of those cases die. Most are elderly. Most had no recent blood tests. Many were on new antibiotics. Many had liver or kidney problems they didn’t know about.
Here’s another hard truth: 15% of theophylline-related problems come from not adjusting for liver disease. 22% come from drug interactions that weren’t caught. That’s not bad luck. That’s poor monitoring.
And yet, some argue theophylline is too risky to use at all. Newer inhalers, biologics - they’re safer. But here’s the catch: biologics cost $200 to $400 a month. Theophylline? $15 to $30. For millions of people in low-resource areas - or even in wealthy countries without good insurance - it’s the only option.

There’s hope on the horizon. Companies like TheraTest Diagnostics and PharmChek Solutions are testing handheld devices that can measure theophylline levels from a finger-prick blood sample in under 5 minutes. Imagine walking into your doctor’s office, getting a quick test, and adjusting your dose before you leave. No lab wait. No delay.
But until those devices are widely available - and proven accurate - the old way still works best. Serum testing. Regularly. Reliably. With context.
Theophylline is not a drug you start and forget. It’s a drug you manage. Every dose change. Every new medication. Every lifestyle shift. Every change in health. Each one changes how your body handles it.
If you’re on theophylline, you need regular blood tests. Not because your doctor doesn’t trust you. Not because you’re being overly cautious. But because your body changes - and the drug doesn’t. The line between life and danger is thin. Monitoring keeps you on the right side of it.
Patients who stick to monitoring report better asthma control. 82% say their symptoms improve when levels stay in range. 68% say the tests are annoying - but necessary. That’s not just opinion. That’s real experience.
The therapeutic range for theophylline is 10 to 20 mg/L (or 10-20 μg/mL). Below 10 mg/L, the drug usually doesn’t provide enough bronchodilation. Above 20 mg/L, the risk of serious side effects - like seizures, irregular heart rhythms, and vomiting - increases sharply. Some patients may respond well to levels between 5 and 15 mg/L, but this is the exception, not the rule.
Initial monitoring should occur 5 days after starting treatment or 3 days after any dose change. For stable patients, check every 6 to 12 months. But high-risk groups need more frequent checks: every 3 to 6 months for patients over 60, every 1 to 3 months for those with heart failure or liver disease, and monthly during pregnancy. Always test after starting or stopping any new medication, changing smoking habits, or after significant alcohol use.
No. Even if you’ve been stable for years, your body changes. Liver function declines with age. New medications can interact. You might start or stop smoking. You might develop heart or kidney issues without symptoms. Theophylline’s narrow window means even small changes can push you into toxicity. Monitoring isn’t about past safety - it’s about current risk.
Many drugs affect theophylline metabolism. Enzyme inhibitors like erythromycin, clarithromycin, ciprofloxacin, cimetidine, and allopurinol can raise levels by 50-100%. Enzyme inducers like carbamazepine, rifampicin, and St. John’s Wort can lower levels by 30-60%. Even over-the-counter supplements and antibiotics can cause dangerous shifts. Always tell your doctor about everything you’re taking - including herbal products.
Yes. Early signs include nausea, vomiting, tremors, restlessness, insomnia, and a fast heartbeat (over 100 bpm). Later signs - like confusion, seizures, or irregular heart rhythms - are medical emergencies. If you experience any of these and are on theophylline, seek help immediately. Don’t wait for a blood test. Symptoms matter just as much as numbers.
Leave a comments