
When a medicine you’ve taken for months suddenly turns your skin into something that looks like a severe burn, you’re not just having a bad reaction-you’re facing one of the most dangerous drug responses in medicine. Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are not common, but when they happen, they can kill. And they don’t come with warning. One day you’re fine. The next, your skin starts peeling off, your eyes burn, your mouth won’t open, and you’re fighting for your life in a hospital bed.
They’re not two separate diseases. They’re two ends of the same deadly spectrum. Think of it like a fever: a low-grade fever is uncomfortable, but a high fever can be life-threatening. SJS and TEN work the same way. The only real difference is how much of your skin is affected.
If less than 10% of your skin detaches, it’s classified as SJS. If more than 30% detaches, it’s TEN. Between 10% and 30%? That’s the overlap form-just as dangerous as either end. The higher the skin loss, the higher the chance you won’t survive. TEN kills about 1 in 4 people who get it. SJS kills about 1 in 10.
It’s not just the skin. Your mucous membranes-inside your mouth, eyes, genitals, and throat-are always involved. In fact, if your mouth isn’t covered in painful blisters and ulcers, it’s probably not SJS or TEN. This isn’t a rash. It’s your body attacking itself.
It starts with a drug. Over 80% of cases are triggered by medications. The rest? Sometimes infections like Mycoplasma pneumoniae, especially in kids. But drugs are the main culprits.
Three medications stand out: carbamazepine (used for seizures and nerve pain), allopurinol (for gout), and sulfonamide antibiotics like Bactrim. Together, they cause more than half of all cases. Lamotrigine, NSAIDs like ibuprofen, and nevirapine (an HIV drug) also show up often.
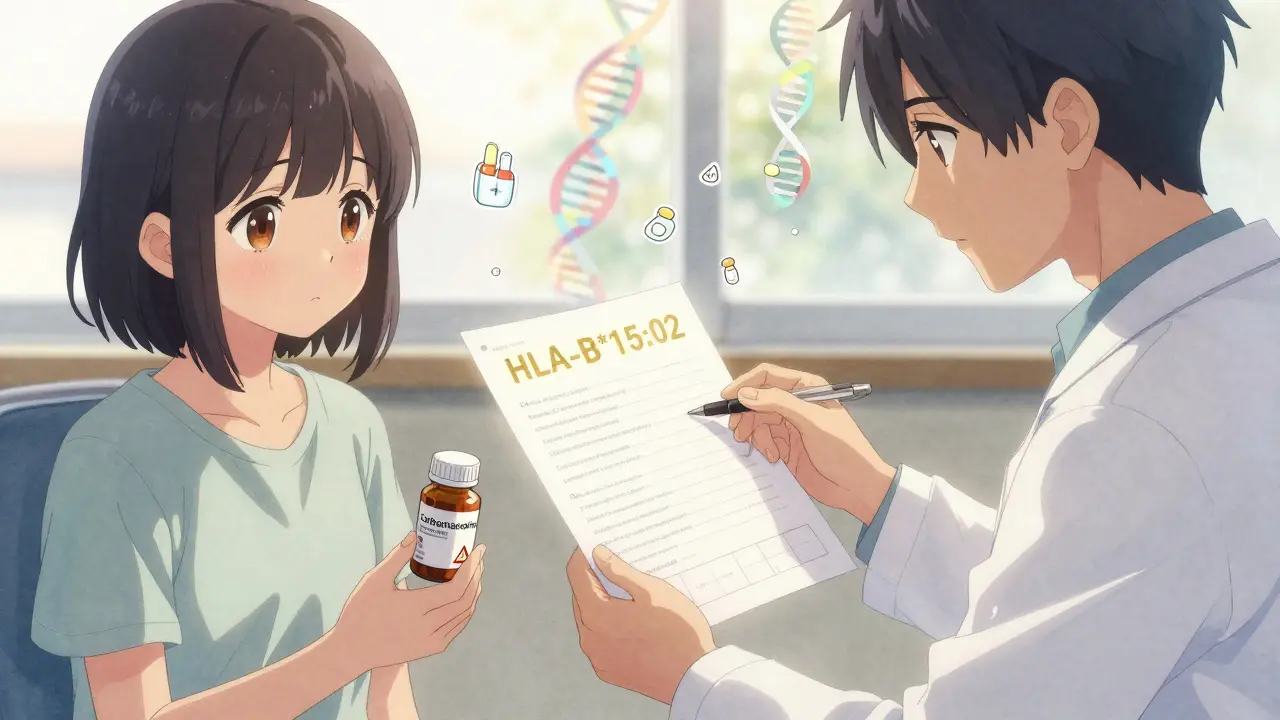
But here’s the twist: not everyone who takes these drugs gets SJS or TEN. Only a tiny fraction do. So why them? Genetics. If you carry the HLA-B*15:02 gene, taking carbamazepine raises your risk by up to 1,000 times. If you have HLA-B*58:01, allopurinol becomes far more dangerous. These aren’t rare genes-they’re common in Asian populations. That’s why countries like Taiwan now require genetic testing before prescribing these drugs. And it’s working. SJS cases dropped by 80% after screening started.
The body’s immune system, confused by the drug, turns on the skin. Immune cells release a toxin called granulysin, which kills skin cells from the inside out. Your epidermis-the outer layer of skin-just peels away. It’s like your skin is melting off.
It doesn’t start with blisters. It starts with a fever, sore throat, burning eyes, and a headache-like the flu. You might think it’s just a bad cold. That’s the trap. This phase lasts 1 to 3 days. Then, the skin changes. Red or purple spots appear, usually on your chest or back. They don’t itch. They hurt. A lot.
Within 24 to 72 hours, those spots turn into blisters. They don’t pop like normal ones. They merge. Sheets of skin start sliding off. If you rub your skin gently and it tears away, that’s the Nikolsky sign-a classic clue doctors look for. Your mouth becomes so painful you can’t eat or drink. Your eyes swell shut. Your genitals burn. You’re in agony.
By day 5 to 8, you’ve lost a huge amount of fluid through your raw skin. Your blood pressure drops. Your kidneys struggle. You’re at risk of sepsis. This isn’t a dermatology case. It’s a burn unit emergency.
There’s no single blood test. No quick scan. Diagnosis comes from three things: your symptoms, your medication history, and a skin biopsy.
The biopsy shows full-thickness death of skin cells-with almost no inflammation in the deeper layers. That’s key. Other skin conditions like staphylococcal scalded skin syndrome look similar, but they affect children and have different tissue patterns. If the biopsy shows widespread keratinocyte death, it’s SJS or TEN.
Doctors also use a scoring tool called SCORTEN. It looks at seven things: your age, whether you have cancer, your heart rate, how much skin is detached, your blood sugar, urea levels, and bicarbonate. Each factor adds to your risk. Three factors? 35% chance of death. Five or more? 90%.
Time matters. The faster you’re diagnosed, the better your odds. Delay by even 24 hours can make a huge difference.
You’re not going to a regular ward. You’re going to a burn unit or ICU. Your skin is like a third-degree burn. You need the same care.
First step: stop every single non-essential drug. Even if you think it’s safe. The culprit might not be obvious. Sometimes it’s a new antibiotic you took last week. Or an over-the-counter painkiller you started for a headache.
Next: fluids. You’re losing liters a day through your skin. You’ll need three to four times the normal amount of IV fluids. Electrolytes are monitored constantly. Your kidneys, liver, lungs-all are under stress.
Wound care is brutal. No sticky bandages. No ointments that trap heat. Non-adherent dressings, sterile gauze, and gentle cleaning. Pain control is critical. You’ll need strong opioids.
Eye care is non-negotiable. Without daily ophthalmology visits, you’re at high risk of permanent damage: dry eyes, scarring, even blindness. Up to 80% of survivors have lasting eye problems.
Antibiotics? Only if there’s clear infection. Using them too early can make things worse.
This is where things get messy. For years, doctors tried everything: steroids, IVIG (intravenous immune globulin), plasma exchange. Most didn’t help.
IVIG was once the go-to. It’s expensive, and you need a lot-2 to 3 grams per kilogram of body weight. But multiple studies now show it doesn’t reduce death rates. It might help in the very early hours, but not later.
Steroids? Risky. They suppress your immune system, which sounds good-but it also makes infections more likely. Some doctors still use high-dose methylprednisolone early on, but evidence is weak.
One treatment that stands out is cyclosporine. In a 2016 trial, patients on cyclosporine had a death rate of 12.5%. Those without it? 33.3%. It blocks the immune cells that are killing your skin. It’s now a top choice in many hospitals.
The most promising new option? Etanercept. It blocks TNF-alpha, a key inflammation driver. In a 2019 study, 12 patients with TEN got etanercept within 48 hours. Zero died. The historical death rate for that group was over 30%. It’s not FDA-approved for this use yet, but it’s being used off-label-and it’s changing outcomes.

Surviving is just the beginning. Sixty to eighty percent of people who make it out of the hospital face lifelong problems.
Your skin won’t look the same. Scarring, dark or light patches, and thinning skin are common. Nails may grow back crooked or fall off. Your genitals might develop scarring that causes pain during sex or urination. Some need surgery to fix urethral strictures or vaginal adhesions.
And your eyes? Even if you don’t go blind, you’ll likely need eye drops for the rest of your life. Dry eyes, light sensitivity, chronic inflammation-they’re almost guaranteed.
Then there’s the mental toll. Forty percent of survivors develop PTSD. The pain, the isolation, the fear of dying, the sight of your own skin peeling off-it haunts people. Many can’t return to work. Relationships suffer. Depression is common.
Recovery takes months. Some need years. And you’ll never be the same.
Yes. And it’s easier than you think.
If you’re of Asian descent and your doctor wants to prescribe carbamazepine, ask for an HLA-B*15:02 test. If you’re over 50 and have gout, and your doctor wants to start allopurinol, ask for HLA-B*58:01 testing. These tests are simple blood draws. Results can come back in hours now-not weeks.
And if you’ve had SJS or TEN once? Never take that drug again. Ever. Even a tiny dose can trigger it again-faster and worse.
Doctors need to stop assuming that if a drug worked for someone else, it’s safe for you. Genetics matter. Race matters. History matters. A simple genetic test can save your life.
Most cases are preventable. We just haven’t made it routine.
Researchers are racing to find more genetic markers. The iSCAR consortium is tracking over 1,200 cases worldwide. They’re looking for patterns-what genes make people vulnerable? What other drugs might be dangerous? And they’re testing new drugs that block granulysin, the toxin that kills your skin cells.
One day, we might have a pill that stops the reaction before it starts. But for now, the best defense is knowledge. Know your meds. Know your genes. Speak up if something feels wrong.
SJS and TEN are rare. But they’re not random. They’re predictable. And if we act early, we can stop them before they start.
Leave a comments