
If you’re allergic to shellfish, eating out isn’t just a risk-it’s a minefield. One bite of shrimp scampi, a splash of fish sauce in your stir-fry, or even fried food cooked in the same oil as crab cakes can trigger a reaction. And it’s not just about the food on your plate. The real danger often comes from what you can’t see: hidden ingredients, shared fryers, and cross-contact that even the most careful kitchen might miss.
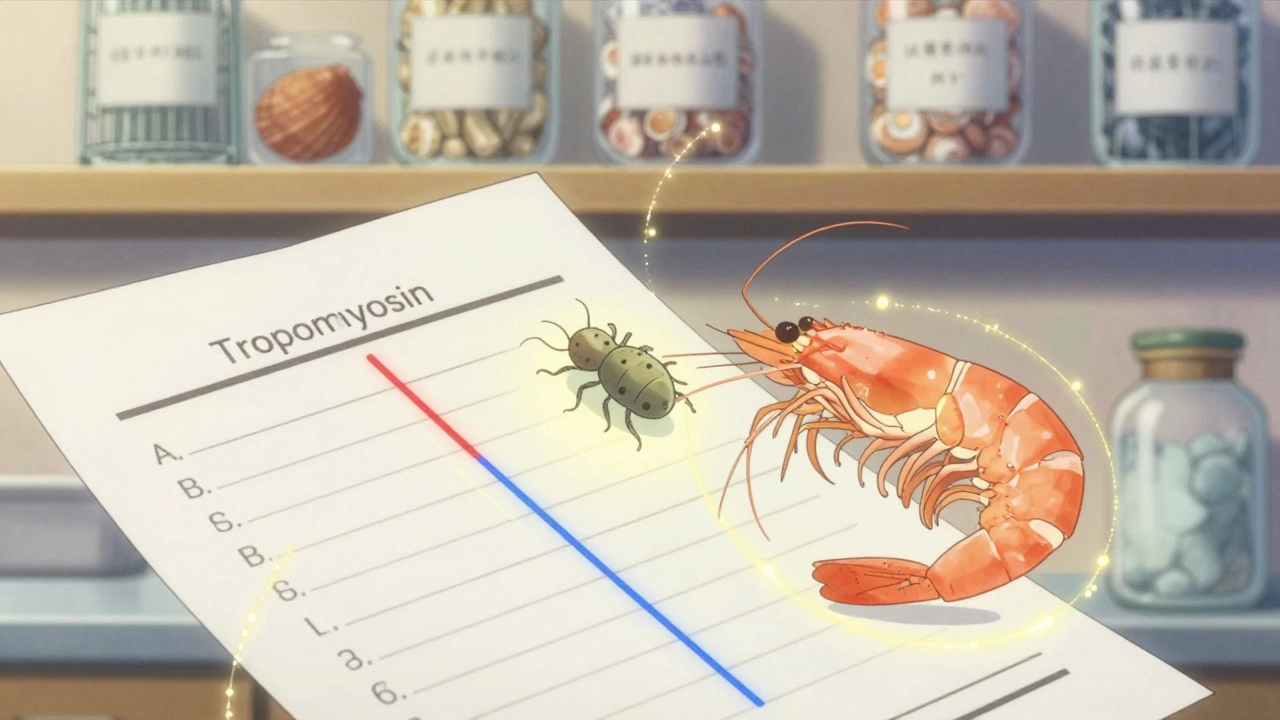
This protein is also found in dust mites and cockroaches. That’s why so many people with shellfish allergies also test positive for mite allergies-even if they’ve never eaten shellfish. A 2025 study showed 68% of people with dust mite allergies had IgE antibodies to shellfish, but only 15% actually had symptoms. This creates a big problem: blood tests can lie. A positive result doesn’t always mean you’ll react to shellfish. That’s why doctors now recommend component-resolved diagnostics-testing specifically for tropomyosin and other key proteins-instead of just using a broad shellfish extract.
Here’s the breakdown:
| From | To | Cross-Reactivity Rate |
|---|---|---|
| Shrimp | Crab | 92% |
| Shrimp | Lobster | 88% |
| Shrimp | Crawfish | 85% |
| Shrimp | Clams | 30-40% |
| Shrimp | Oysters | 25% |
| Shrimp | Scallops | 20% |
That means if you react to shrimp, you might be able to safely eat scallops or oysters-but only if you’ve been properly tested. Many people avoid all shellfish out of fear, when they might only need to avoid crustaceans. A 2020 European study found that component testing allowed 40% of crustacean-allergic patients to safely include mollusks in their diet.
Here’s what most people don’t realize: you don’t need to eat shellfish to react. Cross-contact is the silent killer. If a fryer is used for shrimp, then later for chicken nuggets, the oil still contains allergenic proteins. A 2019 study found that 63% of crustacean reactions happened because of shared fryers. Even a spatula that touched shrimp and then got used on your salad can be enough to trigger symptoms.
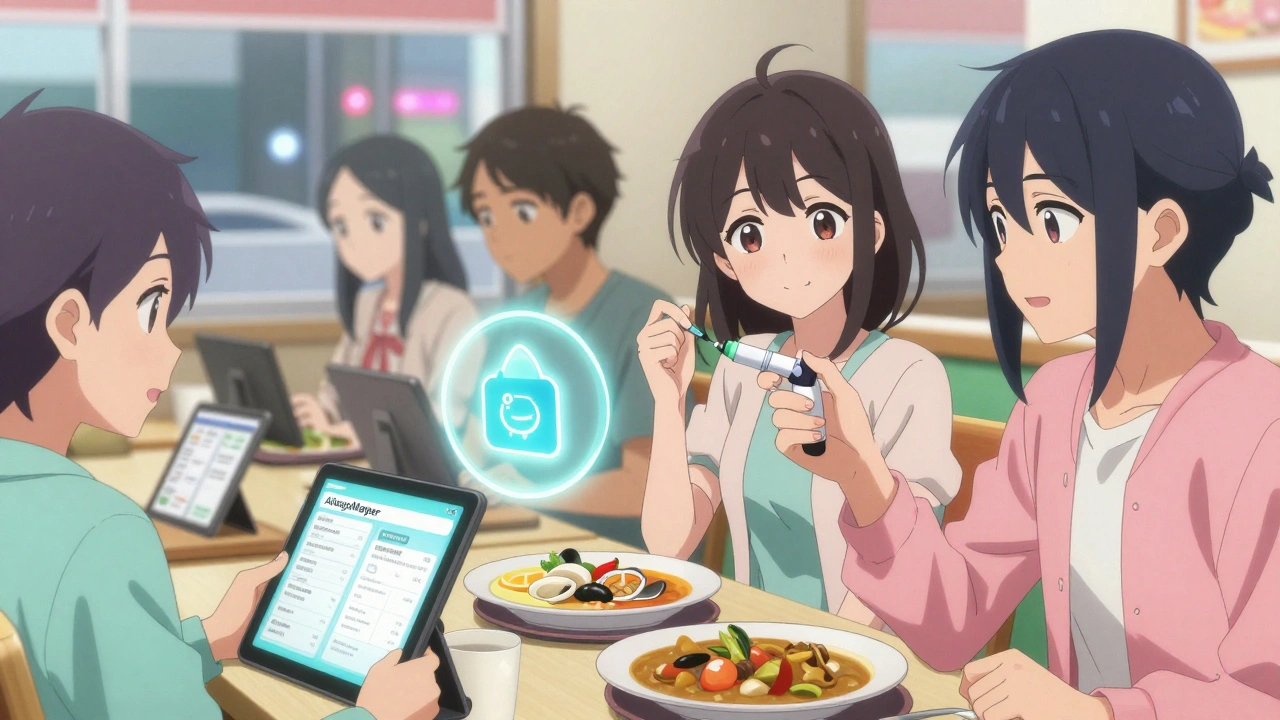
And here’s the kicker: most restaurant staff don’t know what they’re serving. A 2023 National Restaurant Association study found that only 37% of servers could correctly identify shellfish ingredients on the menu. Servers often think “gluten-free” means “safe for allergies,” which is dangerously wrong.
Know the signs: hives, swelling of the lips or throat, wheezing, vomiting, dizziness, or a sudden drop in blood pressure. If you feel any of these, use your epinephrine immediately. Don’t wait. Don’t take an antihistamine first. Epinephrine is the only thing that stops anaphylaxis.
Call 911 after using it. Even if you feel better, you need to be monitored for at least 4-6 hours. A second wave of symptoms can hit hours later.
And there’s hope on the horizon. In early 2024, Phase 2 trials at Mount Sinai showed that peptide immunotherapy for shrimp allergy led to 70% of participants becoming desensitized. They could eat small amounts of shrimp without reaction. It’s not a cure yet, but it’s a major step forward.
Meanwhile, AI tools like AllergyMapper (launched in March 2024) are scanning restaurant menus and flagging hidden shellfish ingredients-like shrimp paste in Thai curry or crab extract in ramen broth-with 85% accuracy. These tools aren’t perfect, but they’re getting better.
Don’t let fear stop you from living. But don’t let ignorance put you in danger. Test properly. Carry your epinephrine. Speak up. And never assume a restaurant knows what’s safe. You’re the expert on your body. Trust yourself.
Unlike peanut or egg allergies, shellfish allergy is rarely outgrown. Only about 10-15% of children with shellfish allergy eventually tolerate it, and even then, it’s usually after years of strict avoidance and supervised testing. For adults, the allergy is typically lifelong. Don’t assume you’ve outgrown it without a doctor-supervised oral food challenge.
No. Imitation crab is made from surimi, which is processed white fish-but it often contains shellfish extracts or is processed on shared equipment. Even if the label says “no shellfish,” cross-contact is common. Always treat it as unsafe unless you’ve confirmed with the manufacturer that it’s produced in a dedicated, allergen-free facility.
No. Shellfish allergy has nothing to do with iodine. That’s an old myth. Reactions to contrast dye are caused by the chemical structure of the dye itself, not by shellfish proteins. People with shellfish allergies are no more likely to react to iodine-based contrast than anyone else. Don’t avoid necessary medical procedures because of this misconception.
It’s risky. Many sushi restaurants use fish sauce, shrimp paste, or crab sticks in sauces and rolls. Even plain sushi rice can be seasoned with dashi made from dried shellfish. If you go, call ahead, ask for a chef card, and request a plain grilled fish or vegetable roll with no sauces. Avoid anything labeled “spicy,” “tempura,” or “special.” And never trust the server’s word-ask to speak to the chef.
You’re not alone. Even restaurants with “allergy-friendly” labels can have lapses. Staff turnover, miscommunication, and pressure during busy hours lead to mistakes. That’s why carrying epinephrine is non-negotiable. If you react, document what you ate, who you spoke to, and what happened. Report it to the restaurant and to organizations like FARE. Your experience helps improve safety for others.
Yes. Peptide immunotherapy for shrimp allergy showed 70% success in early trials, helping patients tolerate small amounts without reaction. Oral immunotherapy trials are also underway. These aren’t cures yet, but they could one day allow people to eat shellfish safely-or at least avoid life-threatening reactions if accidentally exposed. Clinical trials are open in the U.S. and Australia, and more are expected by 2026.
Joe Lam
5 12 25 / 12:36 PMLet’s be real-most restaurants are just glorified germ farms with napkins. I’ve seen servers wipe down tables with the same rag they used to clean the fryer. If you think your ‘allergy-friendly’ sushi spot is safe, you’re one shrimp paste splash away from an EMT call. This isn’t dieting-it’s survival. And no, your ‘I’m careful’ attitude doesn’t make you immune to cross-contact. You’re not special. You’re just lucky so far.
jagdish kumar
6 12 25 / 05:13 AMThe shellfish is not the enemy. The fear is. We are all just dust mites in a larger soup. Tropomyosin? It is the same as the silence between heartbeats. You think you control your life by avoiding shrimp. But the ocean remembers. And the ocean is always hungry.
zac grant
7 12 25 / 23:31 PMReally glad this post broke down component-resolved diagnostics-it’s still massively underutilized. Most allergists still rely on IgE panel tests that give you false positives because of tropomyosin cross-reactivity with mites. The ImmunoCAP ISAC 112 panel? Game-changer. If you’re allergic to shrimp but have no symptoms with scallops, don’t assume you’re just ‘being paranoid.’ Get tested for penaeidin and arginine kinase. You might be able to expand your diet safely. Also, AllergyEats is legit-used it in Austin last month and found a Thai place with a dedicated fryer. Mind blown.
Pavan Kankala
9 12 25 / 23:25 PM98% accuracy on those chain allergen menus? LOL. Did you know Starbucks uses the same steamer for oat milk and dairy? And they call it ‘allergen-free’? The FDA’s just a front for Big Food. They want you to think you’re safe so you keep buying. That ‘peptide immunotherapy’? Probably funded by shrimp conglomerates. They’re not curing you-they’re conditioning you to eat more of it slowly until you’re hooked. Wake up. They’re selling you a false sense of security so you’ll keep dining out. And when you collapse in the middle of Chipotle, who gets sued? You do.
Jessica Baydowicz
10 12 25 / 08:35 AMY’all. I used to avoid EVERYTHING because I was terrified. Then I got a chef card (FARE’s one, in Spanish-I travel a lot), called ahead religiously, and found this tiny taco joint in San Diego where the owner literally hand-wrote my allergy on the menu board. He even made me a separate batch of guac with a clean spoon. I cried. Like, ugly cried. You CAN eat out. It’s not about fear. It’s about finding your people. And they’re out there. You just gotta ask. 💛
John Filby
11 12 25 / 01:26 AMJust wanted to say I’ve been shellfish-allergic since I was 5 and now I’m 32 and still alive 😅. The chef card thing is 100% legit-I carry it in my wallet and in my phone. Also, I found out I’m fine with scallops after a supervised oral challenge. No one told me that was even an option. If you’re scared, talk to an allergist who does component testing. It’s not just a blood test-it’s your freedom ticket. And yes, carry two epinephrine pens. I’ve used mine twice. It’s scary, but it works. 🙏
Elizabeth Crutchfield
11 12 25 / 22:45 PMi just had a reaction last month at a ‘gluten free’ pizza place and i was like… wait… they used shrimp in the broth for the crust?? i thought gluten free meant safe?? now i just call every place and say ‘i have a life or death allergy’ and they usually get it. but i still panic every time. i carry my epi like a charm. also… why is everyone so nice to me now that i say ‘life or death’??
Rachel Bonaparte
13 12 25 / 16:31 PMLet’s not pretend this is just about food. This is about power. The food industry doesn’t want you to know that tropomyosin is stable at 400°C because if you did, you’d realize that ‘grilled’ doesn’t mean ‘safe.’ They want you to believe that ‘allergy-friendly’ is a label you can trust. It’s not. It’s marketing. The FDA approved the ImmunoCAP ISAC 112 panel? Sure. But did you know they didn’t require restaurants to disclose cross-contact risks? That’s not oversight-that’s negligence. And the AI tools? AllergyMapper? They’re trained on data from chains that have dedicated fryers. What about the 90% of mom-and-pop places? You think they’re scanning menus? No. They’re just hoping you don’t die. And if you do? They’ll say ‘we didn’t know.’ Well, now you know. And now you’re responsible for your own survival. Welcome to capitalism, sweetheart.
Scott van Haastrecht
13 12 25 / 19:12 PMSo let me get this straight-you’re telling me the solution to a life-threatening allergy is to call a restaurant, ask for the chef, and pray they don’t screw up? And if they do, you’re supposed to inject yourself with epinephrine and wait for an ambulance? That’s not safety. That’s Russian roulette with a side of miso soup. The fact that we’ve normalized this as ‘responsible behavior’ is the real tragedy. We’ve turned medical necessity into a performance art. And the worst part? The people who die? They didn’t fail. The system did. This post is just a glorified survival guide for a world that refuses to fix the problem. So go ahead. Carry two pens. Call ahead. Use the app. But don’t pretend you’re in control. You’re just delaying the inevitable.