
When a cough turns into fever and breathing feels heavy, many people wonder what’s really happening inside their lungs. Understanding the pneumonia puzzle-what sparks it and how it shows up-helps you act fast and avoid complications.
Pneumonia is an inflammatory infection of the lung tissue that fills the air sacs with fluid or pus, causing cough, fever, chills, and difficulty breathing. It can be triggered by different microbes, inhaled substances, or even a weakened immune system. The condition ranges from mild, treatable cases to severe, life‑threatening bouts that need hospital care.
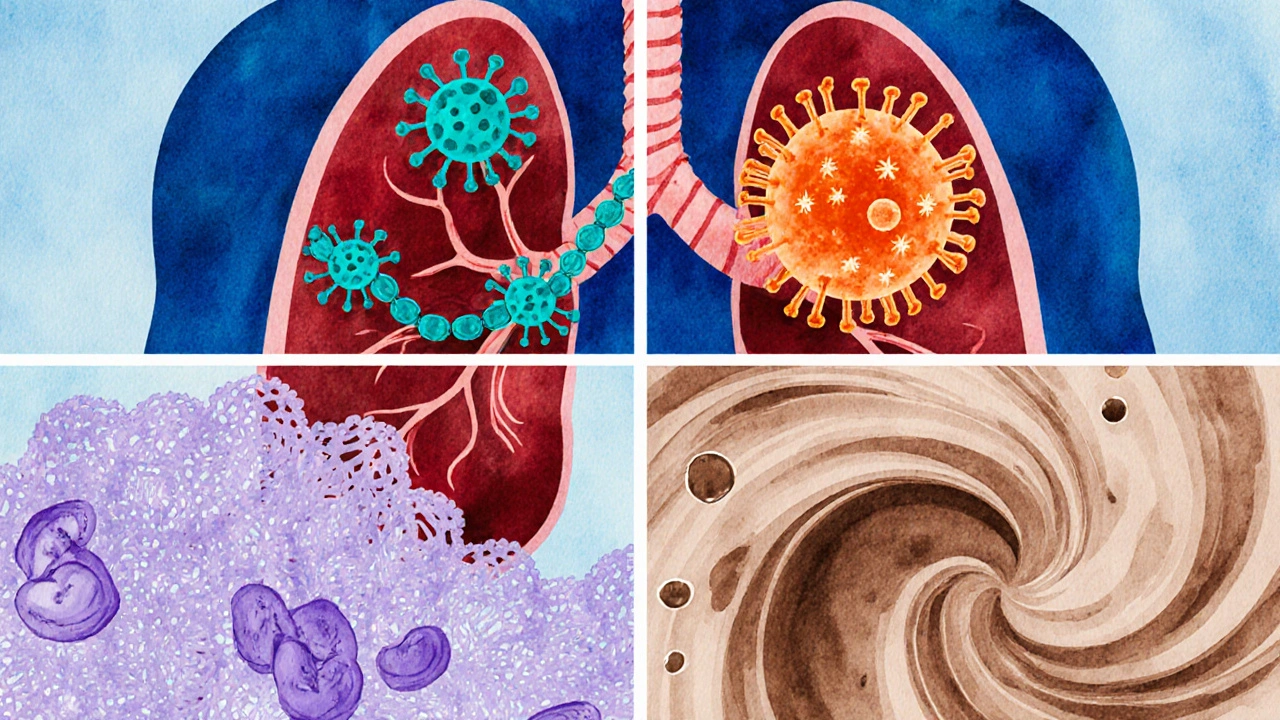
The three big families that cause pneumonia are bacteria, viruses, and fungi. A fourth, less talked about cause is aspiration-food, drinks, or vomit entering the lungs.
Bacteria are single‑cell microorganisms that multiply rapidly and often cause the most classic, sudden‑onset pneumonia. Typical bacterial culprits release toxins that inflame the alveoli, leading to a rapid buildup of fluid.
Viruses invade lung cells, hijack their machinery, and trigger an immune response that fills the air sacs with inflammatory fluid. Viral pneumonia often follows a cold or flu and may progress more gradually.
Fungi are less common but can cause chronic, slowly progressing lung infection, especially in people with weakened immune systems.
Aspiration occurs when food, saliva, or gastric contents are inhaled, bringing bacteria from the mouth into the lungs and sparking an inflammatory reaction.
Symptoms can vary by cause, age, and overall health, but most people notice a handful of classic signs:
Diagnosis blends a physical exam with imaging and lab tests. The most common imaging tool is the chest X‑ray.
Chest X‑ray provides a quick snapshot of the lungs, showing areas of consolidation (white patches) that indicate fluid‑filled air sacs. In severe cases, a CT scan may be ordered for more detail.
Blood tests-including C‑reactive protein (CRP) and white‑blood‑cell count-help gauge inflammation. Sputum culture identifies the exact microbe, guiding targeted therapy.
Anyone can catch pneumonia, but certain groups face higher odds:
The right treatment depends on the cause.
Hospital admission is required when patients show severe breathing difficulty, low oxygen saturation, or complications like sepsis.

Many cases of pneumonia can be avoided with simple steps:
| Cause Type | Typical Pathogen | Onset Speed | First‑Line Treatment |
|---|---|---|---|
| Bacterial | Streptococcus pneumoniae | Sudden, within 1-3 days | Antibiotics (e.g., amoxicillin) |
| Viral | Influenza virus | Gradual, 3-7 days after flu symptoms | Antivirals if early; otherwise supportive care |
| Fungal | Pneumocystis jirovecii | Slow, weeks to months | Antifungal agents (e.g., TMP‑SMX) |
| Aspiration | Mixed oral flora | Variable, often after choking event | Broad‑spectrum antibiotics + airway clearance |
Yes. The germs that cause pneumonia-especially viruses and bacteria-can spread through droplets when an infected person coughs or sneezes. Close contact, shared utensils, or touching contaminated surfaces can also transmit the microbes.
Mild bacterial cases often improve within 5-7 days of antibiotics. Viral pneumonia may linger for 2-3 weeks, especially if fatigue remains. Severe infections that require hospitalization can take several weeks to fully resolve.
A chest X‑ray is the standard first test because it quickly confirms lung involvement. However, in very mild cases where the clinical picture is clear, doctors may start treatment based on symptoms alone and reserve imaging for uncertainty.
No. The flu vaccine contains inactivated or recombinant virus particles that cannot cause infection. In fact, getting the flu shot reduces the chance of developing viral pneumonia linked to influenza.
Stay hydrated, use a humidifier, rest plenty, and take over‑the‑counter fever reducers like ibuprofen. Warm liquids (broths, herbal teas) can soothe a sore throat and ease cough.
Neil Greer
14 10 25 / 19:24 PMHey folks, great rundown on pneumonia! I love how you broke down the different causes – makes it way easier to spot what might be going on. Gotta say, the table comparison is super handy for quick reference. Keep the info coming, it really helps us stay on top of our health.
Fionnuala O'Connor
15 10 25 / 14:51 PMThis is really helpful. The way you listed the vaccines at the end is clear and I can remember it easily.
Adam O'Rourke
16 10 25 / 10:17 AMWow, another super‑serious medical article – just what I needed while scrolling through memes :) But seriously, you could've mentioned that not every cough means pneumonia, you know?
Mary-Pat Quilty
16 10 25 / 11:41 AMAh, the drama of tiny microbes invading our lungs! Imagine the battle – bacteria like relentless warriors, viruses as sly infiltrators, and fungi as the slow‑burn villains. It's a theatrical showdown right inside our chests, and the symptoms are the tragic cries of the body pleading for aid. Your table paints this epic saga perfectly, turning a medical lecture into a saga worthy of the stage.
Patrick McGonigle
17 10 25 / 09:54 AMThe article does a solid job explaining the major pathogens. Streptococcus pneumoniae remains the most common bacterial cause, and the flu virus leads viral cases during flu season. Treatment recommendations are clear – antibiotics for bacterial, antivirals for influenza‑related cases. Overall, the information is concise and accurate.
Keisha Moss Buynitzky
17 10 25 / 11:01 AMDear readers, I appreciate the thoroughness of the previous comment. It is essential to recognize that early diagnosis can dramatically improve outcomes, especially in vulnerable populations. Please consider following up with your healthcare provider if symptoms persist.
Shivam yadav
18 10 25 / 09:14 AMNice content! I think it’s cool how you highlighted both vaccination and lifestyle changes. It shows that prevention is a shared responsibility, not just something doctors do.
pallabi banerjee
18 10 25 / 10:04 AMIndeed, the balance between medical intervention and personal habits is crucial. When we maintain good hygiene and manage chronic conditions, we reduce the risk of infection. This article reminds us of that holistic perspective.
Brittaney Phelps
19 10 25 / 05:31 AMGreat summary! Quick tip: stay hydrated when you’re sick – it helps thin secretions.
Kim Nguyệt Lệ
19 10 25 / 06:54 AMTypo alert: "pneumonia" was misspelled as "pnemonia" in the opening paragraph. Otherwise, the content is accurate.
Rhonda Adams
20 10 25 / 02:21 AMLoved the depth of this guide! It really clears up a lot of confusion 😊 Keep up the good work!
Macy-Lynn Lytsman Piernbaum
20 10 25 / 21:47 PMThanks for the info! 🌟 It’s awesome to see the breakdown of symptoms – makes it easier to know when to seek help.
Richard Phelan
20 10 25 / 22:37 PMAh, the grand finale of medical prose! Your article stands as a beacon of clarity amidst the fog of confusion. It dazzles with data and delights with detail, truly a masterpiece of healthcare narration.
George Kata
21 10 25 / 20:51 PMWell written, and I appreciate the balanced tone. The mix of formal and casual language makes it approachable for everyone.
Nick Moore
21 10 25 / 22:14 PMExcellent stuff!
Sriram Musk
22 10 25 / 20:27 PMReading through this article feels like taking a guided tour through the complex world of respiratory infections. First, it establishes a clear definition of pneumonia, reminding us that it is an inflammatory infection that fills alveoli with fluid or pus. Then it categorizes the primary causes – bacteria, viruses, fungi, and aspiration – which sets the stage for deeper understanding. The discussion of specific pathogens, such as Streptococcus pneumoniae and Haemophilus influenzae, provides concrete examples that readers can recognize. Moving on, the symptom list is thorough, covering everything from cough and fever to chest pain and tachycardia, which helps individuals self‑identify potential cases.
Diagnosis methods are explained concisely, emphasizing the role of chest X‑rays, CT scans, and lab tests like CRP and sputum cultures. The risk factor section is comprehensive, highlighting age groups, chronic lung disease, smoking, alcohol use, and immunocompromised states. Treatment options are broken down by cause, noting antibiotics for bacterial cases, antivirals for influenza, antifungals for fungal infections, and supportive care across the board. The article also wisely points out when hospitalization becomes necessary, such as severe dyspnea or sepsis.
Prevention strategies are practical: vaccinations, hand hygiene, smoking cessation, and chronic disease management. The comparison table succinctly contrasts bacterial, viral, fungal, and aspiration pneumonias, making it easy to remember onset speed and first‑line therapy. Finally, the FAQ section anticipates common concerns, clarifying transmission, recovery timelines, imaging necessity, vaccine safety, and home remedies. Overall, the piece is well‑structured, evidence‑based, and accessible, offering readers a valuable resource for both education and practical guidance.