Getting the right dose of medicine for a child isn’t just about guessing based on age. It’s a life-or-death math problem. One wrong decimal, one missed conversion, and a safe dose becomes dangerous-sometimes fatally so. In pediatric care, weight-based dosing isn’t just best practice; it’s the only reliable way to prevent harm. For every child, the dose must match their body weight, not their birthday. And even then, you can’t stop there. You need a second pair of eyes.
Why Weight Matters More Than Age
Kids aren’t small adults. Their bodies process drugs differently. A newborn’s liver and kidneys aren’t fully developed. A toddler’s body water percentage is higher than an adult’s. A teenager’s metabolism can change overnight. That’s why age-based dosing-like ‘give half a teaspoon for ages 2-5’-is risky. Research shows it leads to errors in nearly 3 out of 10 cases, especially in kids who are smaller or larger than average.
Weight-based dosing fixes this. It uses the child’s actual weight in kilograms to calculate the exact amount of medicine. For example, amoxicillin for ear infections is often dosed at 40-90 mg per kg per day. If a child weighs 15 kg, that’s 600-1,350 mg total per day. Split into two doses? That’s 300-675 mg per dose. Simple. Precise. Safe.
The Three-Step Formula You Can’t Skip
There’s a reason hospitals train nurses and doctors to follow this exact sequence:
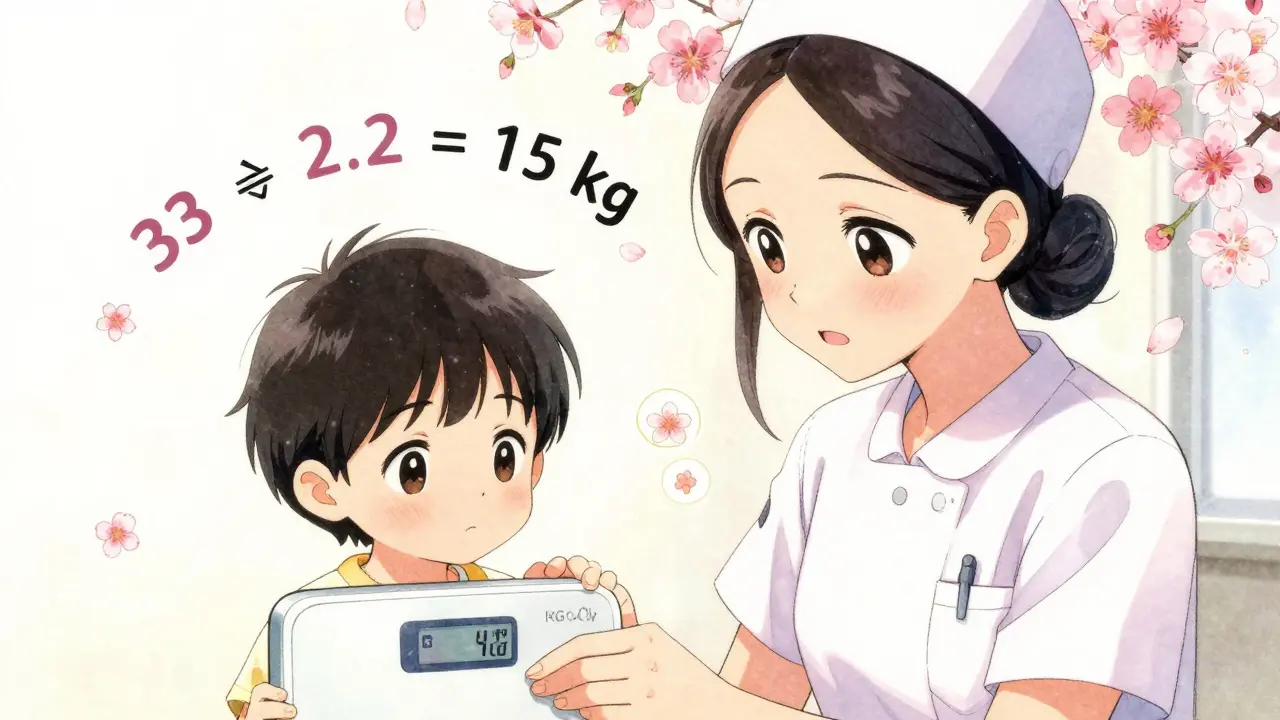
- Convert pounds to kilograms. Use the exact conversion: 1 kg = 2.2 lb. Never round until the final step. A 33-pound child is 15 kg (33 ÷ 2.2), not 15.5 or 14.9. Rounding too early adds error.
- Multiply weight by the dose per kg. If the order says 15 mg/kg/day and the child weighs 15 kg, the total daily dose is 225 mg.
- Divide by frequency. If it’s given twice a day, each dose is 112.5 mg. Don’t guess-calculate.
A real mistake happened last year at a community hospital in Texas. A 22-pound (10 kg) child was prescribed 40 mg/kg/day of vancomycin. The nurse calculated 400 mg total per day but forgot to divide by two. The child got 400 mg in one dose-double the safe amount. They recovered, but only because the pharmacist caught it during final review. That’s why step three isn’t optional.
When Weight Isn’t Enough: Special Cases
Not all kids fit the standard model. For children with obesity-especially those above the 95th percentile for BMI-using actual body weight can lead to overdosing. That’s because fat tissue doesn’t absorb water-soluble drugs like antibiotics or painkillers the same way muscle does.
In these cases, hospitals use
adjusted body weight:
Adjusted Body Weight = Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight)
This method is now standard in 78% of children’s hospitals, according to the Children’s Hospital Association. For example, a child who weighs 50 kg but has an ideal weight of 30 kg would have an adjusted weight of 38 kg. That changes the dose significantly.
For chemotherapy drugs, body surface area (BSA) is sometimes used instead. The Mosteller formula-√(weight in kg × height in cm ÷ 3600)-is more accurate for these drugs. But it takes longer. One study found it adds 47 seconds per dose. That’s why weight-based dosing remains the default for most medications.

The Double-Check That Saves Lives
Calculating the dose is only half the job. The other half is verifying it. The American College of Clinical Pharmacy found that independent double-checks reduce serious medication errors by 68% in children.
Here’s how it works in practice:
- One provider calculates the dose based on weight.
- A second provider recalculates it independently-no peeking.
- Both compare results. If they don’t match, they stop and find the error.
This isn’t just policy-it’s law. The Joint Commission’s National Patient Safety Goal requires double-checks for high-alert medications like insulin, opioids, and chemotherapy drugs in pediatric patients.
A nurse in Colorado shared a story on AllNurses: ‘We caught a 10-fold error last month. The resident ordered 200 mg for a 10 kg child. The max safe dose is 40 mg/kg/day-that’s 400 mg total. The nurse calculated 20 mg per dose, not 200. The double-check flagged it immediately.’
Where Things Go Wrong
The Institute for Safe Medication Practices tracked over 1,200 pediatric dosing errors in 2022. The top causes:
- Unit confusion (38%): Mixing pounds and kilograms. One nurse wrote ‘22 lb’ on the chart. The next person read it as ‘22 kg’ and gave 2.2 times the dose.
- Decimal errors (27%): Writing ‘5.0 mg’ instead of ‘50 mg’-or vice versa.
- Ignoring organ function (19%): Giving aminoglycosides to a preterm infant without reducing the dose. Their kidneys can’t clear the drug fast enough.
Hospitals have fought back with simple fixes: red stickers on scales that say ‘WEIGH IN KG ONLY,’ automated alerts in electronic health records that flag doses outside expected ranges, and mandatory annual competency tests for all staff who handle pediatric meds.

Technology Is Helping-But Not Replacing Humans
Epic Systems and other EHR vendors now have built-in pediatric dosing calculators. They auto-convert weight, apply institutional limits, and block unsafe doses. In 78% of children’s hospitals, these tools are standard.
But here’s the catch: technology can’t replace human judgment. A 2023 study showed that 41% of EHR alerts were overridden because the provider thought the system was ‘wrong.’ Turns out, the system was right-the provider had forgotten the child had kidney impairment.
That’s why double-checks still matter. Even with tech, two people must verify.
What You Need to Remember
- Always use kilograms. Never pounds.
- Round only after the final calculation.
- Double-check every high-alert medication.
- Adjust for obesity, prematurity, and organ dysfunction.
- Never assume a dose is safe just because it looks ‘right.’
The goal isn’t perfection. It’s prevention. One mistake can change a family’s life forever. But with careful math and a second set of eyes, we can make sure that doesn’t happen.
Why is weight-based dosing better than age-based dosing for children?
Weight-based dosing is more accurate because children’s bodies process drugs differently based on their size, not their age. A 2-year-old who weighs 30 pounds and one who weighs 18 pounds need different doses, even if they’re the same age. Age-based dosing ignores this and leads to errors in nearly 30% of cases, especially in children at the extremes of growth. Weight-based dosing reduces medication errors by 43% compared to age-based methods, according to the American Academy of Pediatrics.
How do you convert a child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, a 44-pound child is 20 kg (44 ÷ 2.2). Never round the result until after you’ve completed the full dose calculation. Rounding too early can lead to cumulative errors. Always use the exact conversion factor-2.2 lb = 1 kg-and record weight to the nearest hundredth of a kilogram for precision.
What is a double-check protocol in pediatric dosing?
A double-check protocol means two qualified healthcare providers independently calculate and verify the same dose before administration. One person calculates the dose based on the child’s weight and the prescribed mg/kg. The second person recalculates without seeing the first person’s work. If the numbers don’t match, they stop and investigate. This process reduces serious medication errors by 68% in children, according to the American College of Clinical Pharmacy.
Do obese children need special dosing considerations?
Yes. For water-soluble drugs like antibiotics, using actual body weight can lead to overdosing because fat tissue doesn’t absorb these drugs the same way muscle does. Instead, use adjusted body weight: Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight). This method is used in 78% of children’s hospitals. For fat-soluble drugs like some painkillers, actual weight may still be appropriate. Always check institutional guidelines and consult a pharmacist.
What are the most common dosing errors in pediatric care?
The top three errors are: unit confusion (mixing pounds and kilograms-38% of errors), decimal point mistakes (27%), and failing to adjust for kidney or liver problems (19%). Many of these are preventable with proper training, standardized weight measurement in kilograms only, and mandatory double-checks for high-alert medications. The Institute for Safe Medication Practices reports that 92% of pediatric teaching hospitals now use ‘KG ONLY’ labels on scales to prevent unit errors.
Is body surface area (BSA) dosing better than weight-based dosing?
For certain drugs-especially chemotherapy-BSA dosing is more accurate because it accounts for both weight and height. The Mosteller formula (√[weight kg × height cm ÷ 3600]) is used in these cases. However, BSA dosing requires an extra measurement (height) and takes about 47 seconds longer per dose. For most other medications, weight-based dosing is simpler, faster, and just as effective. That’s why it remains the standard for 87% of pediatric doses in hospitals.


Joni O
18 01 26 / 16:05 PMJust wanted to say thank you for this. I’m a pediatric nurse and we do double-checks religiously-it’s exhausting but worth it. Saw a kid almost get 10x the vancomycin dose last month because the resident typed ‘200’ instead of ‘20’. We caught it. God bless the second pair of eyes.
Pat Dean
19 01 26 / 08:49 AMOf course you people care about ‘weight-based dosing’-but what about the fact that 70% of these kids are on Medicaid and their parents can’t even read the labels? This isn’t a math problem, it’s a class problem.
Ryan Otto
21 01 26 / 08:23 AMLet’s not pretend this is about safety. The entire pediatric dosing paradigm is a construct of pharmaceutical lobbying. Weight-based calculations were pushed because they allow for higher drug volumes-and thus, higher profits. The ‘double-check’ is theater. Real safety would mean reducing polypharmacy, not optimizing overdoses.
rachel bellet
23 01 26 / 02:01 AMAs a clinical pharmacist, I’m appalled by the continued reliance on manual calculations. EHRs have built-in decision support with real-time renal/hepatic adjustment flags. The fact that 41% of alerts are overridden isn’t clinician error-it’s systemic burnout and cognitive overload. We’re asking nurses to be pharmacists while they’re staffing at 1:8 ratios. This isn’t a dosing issue-it’s a staffing crisis dressed up as protocol.
And yes, adjusted body weight for obesity? Still underutilized. But you won’t fix it until you stop treating clinicians like calculators.
Jay Clarke
24 01 26 / 13:19 PMOkay but like… imagine if your kid got the wrong dose because someone didn’t divide by two? That’s not a mistake-that’s a moral failure. I’m not even mad, I’m just… heartbroken for the families who’ve been through this. And then you read about some hospital that still uses ‘pounds’ on the chart? That’s not negligence. That’s evil.
Selina Warren
24 01 26 / 20:36 PMTHIS. RIGHT HERE. This is why I became a nurse. Not for the pay. Not for the hours. But for the moments when you catch the error before it’s too late. That Colorado nurse? She’s a hero. And every single person who double-checks-even when they’re tired, even when they’re late-is a quiet warrior. We don’t get trophies. But we save lives. Keep going.
Robert Davis
26 01 26 / 20:14 PMInteresting. I read this whole thing. I’m not sure I agree with anything. I mean, why do we even use kilograms? The metric system is a globalist plot to erase American tradition. And who decided kids shouldn’t be dosed by age? My cousin’s kid got amoxicillin by age chart and turned out fine. Maybe we’re overcomplicating this.
Also, is that EHR software made by Epic? I heard they’re owned by the CIA.
Eric Gebeke
27 01 26 / 16:42 PMThey say ‘double-check’ but they don’t say who’s doing the checking. What if the second person is just as incompetent? What if they’re rushing? What if they’re on their phone? This whole system is built on trust-and trust is a luxury in a broken system. We’re just pretending we’re safe while the real problem-underfunded hospitals, overworked staff, zero accountability-is ignored.
And don’t even get me started on the ‘KG ONLY’ stickers. Cute. But if the scale’s broken and no one fixes it? You’re just decorating the coffin.
Andrew Short
27 01 26 / 17:30 PMLet’s be real-this isn’t about safety. It’s about liability. Hospitals push these protocols because they’re scared of lawsuits, not because they care about kids. The ‘double-check’? It’s a legal shield, not a medical one. And don’t tell me about ‘68% reduction’-correlation isn’t causation. They could’ve just been lucky.
Meanwhile, the real killers? Antibiotic overuse. Poor nutrition. Environmental toxins. But nah, let’s focus on whether someone rounded 15.4 to 15. That’s the real crisis.
Danny Gray
29 01 26 / 04:21 AMWhat if the problem isn’t dosing… but the assumption that children need drugs at all? We’ve medicalized childhood. Ear infections? Often viral. Pain? Maybe they just need cuddles. What if the real danger isn’t the math-but the culture that says every ache needs a pill? Maybe the solution isn’t better calculations… but fewer prescriptions.
And who decided weight was the only variable? What about genetics? Gut microbiome? Epigenetics? We’re reducing human biology to a spreadsheet. That’s not science. That’s reductionist arrogance.
Tyler Myers
30 01 26 / 14:26 PMSo let me get this straight-kids are getting overdosed because someone forgot to divide by two? But the same system that can’t do basic math somehow tracks every kid’s vaccination history, social security number, and what they ate for lunch? This isn’t incompetence. It’s sabotage. Someone’s profit margin depends on you not catching these errors.
And why is it always ‘pediatric’? Why not adult dosing? Oh right-adults don’t have parents to sue. That’s the real story.
Jake Moore
30 01 26 / 22:38 PMJust wanted to add a real-world tip: Always write the weight in kg on the whiteboard next to the bed. Even if the chart says 22 lb, write ‘10 kg’ in big letters. I’ve seen families catch their own kid’s error because they saw it there. Simple. Free. Life-saving. And if you’re ever unsure? Call pharmacy. They don’t mind. They’d rather you call 10 times than miss once.