Enter your thyroid and statin information to calculate your risk of statin-induced muscle damage.
If you’re taking statins for high cholesterol and also have hypothyroidism, you’re at a higher risk for muscle damage - not just mild soreness, but something serious like rhabdomyolysis. This isn’t theoretical. Real people end up in the hospital because their thyroid wasn’t properly managed while on statins. The good news? This risk is mostly preventable.
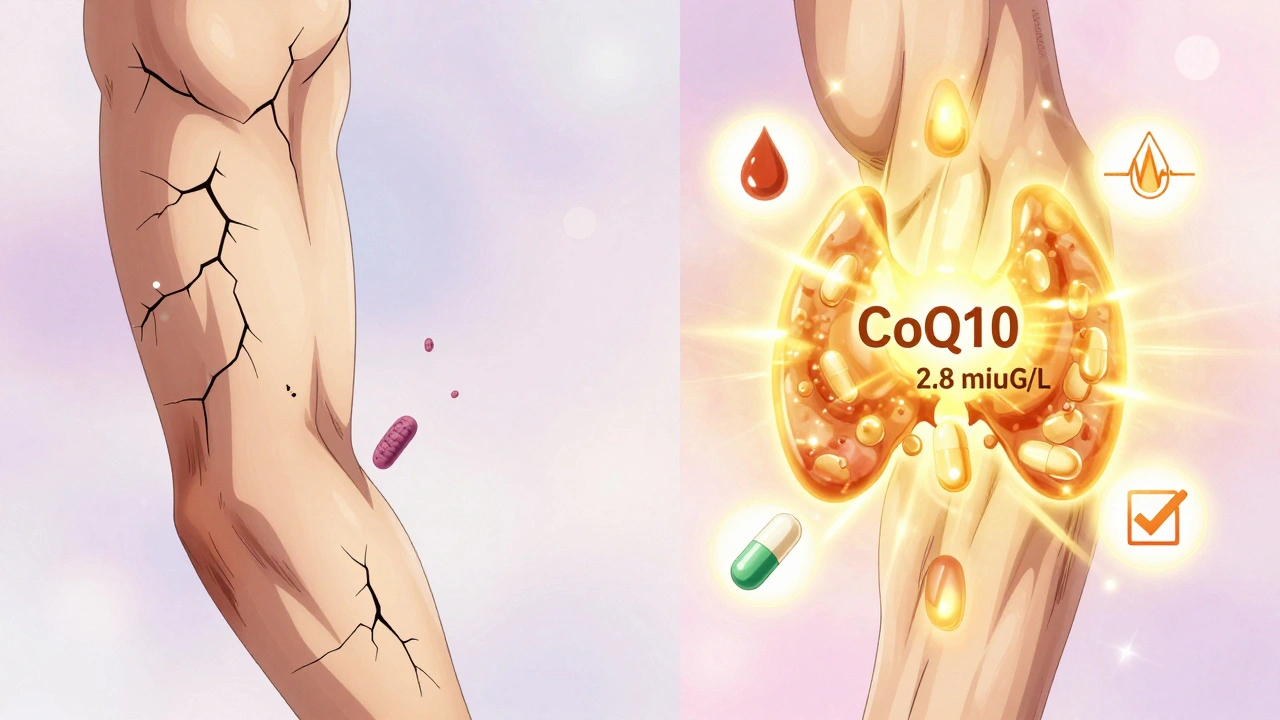
Statins work by lowering LDL cholesterol, but they also interfere with muscle cell energy production. Hypothyroidism does the same thing - slower metabolism, weaker mitochondria, less coenzyme Q10. When you put them together, your muscles get hit from both sides. The result? Muscle pain, weakness, and in extreme cases, kidney failure from muscle breakdown products flooding your system.
It’s not just coincidence. Research shows hypothyroid patients on statins have 3 to 4 times the risk of muscle injury compared to people with normal thyroid function. One study of over 12,000 patients found that those with TSH levels above 10 mIU/L had more than four times the chance of developing statin-induced myopathy. Even subclinical hypothyroidism - where TSH is between 4.5 and 10 - still raises the risk by more than double.
Here’s why: your liver uses enzymes like CYP3A4 to break down statins. In hypothyroidism, these enzymes slow down. That means your body can’t clear the drug fast enough. Atorvastatin and simvastatin, which rely heavily on CYP3A4, build up in your blood by 30-50%. Higher blood levels = higher chance of muscle toxicity.
At the same time, hypothyroidism lowers your body’s natural production of coenzyme Q10 - a compound your muscles need to make energy. Statins also reduce CoQ10 by 25-50%. So you’re getting hit with a double whammy: less fuel and less ability to clean up the drug.
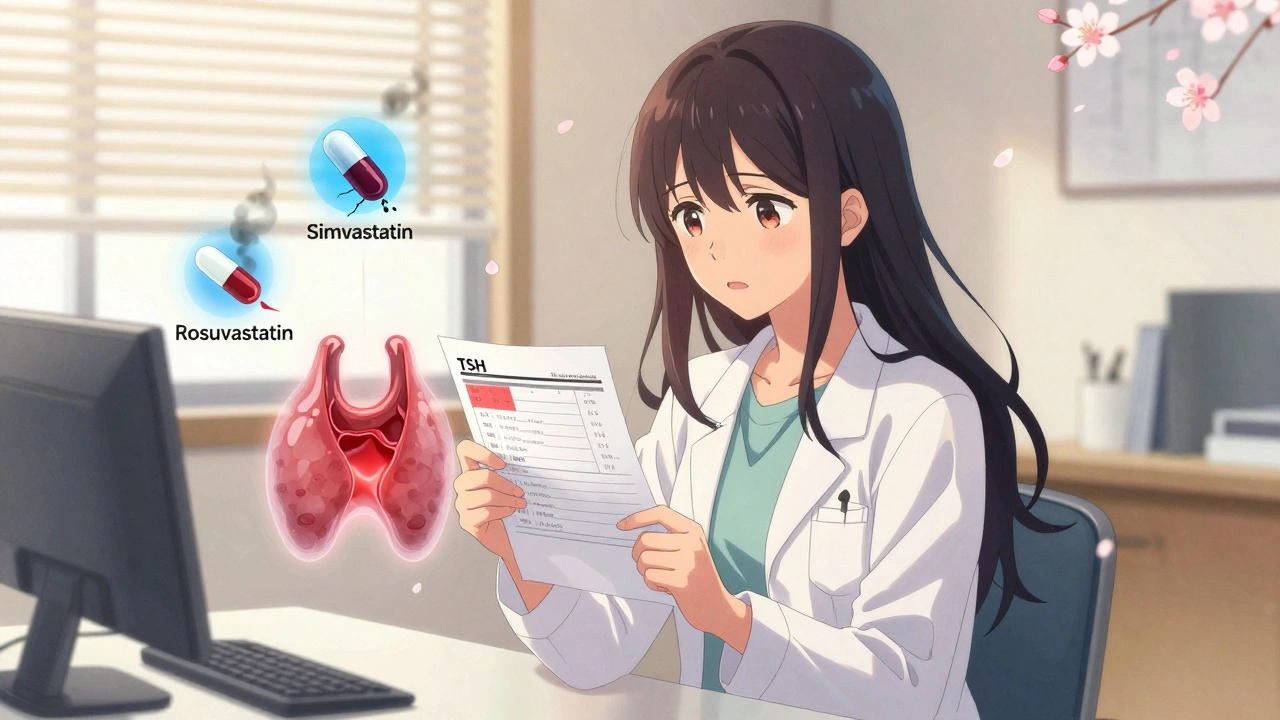
If you have hypothyroidism, the type of statin you take matters a lot. Lipophilic statins - like simvastatin, lovastatin, and atorvastatin - easily slip into muscle cells, increasing damage risk. Hydrophilic statins - like pravastatin and rosuvastatin - stay mostly in the bloodstream and are much gentler on muscles.
Here’s what the data says:
| Statin | Type | Myopathy Risk in Hypothyroid Patients | Recommended Dose |
|---|---|---|---|
| Simvastatin | Lipophilic | 12.7% | Avoid ≥40 mg/day |
| Atorvastatin | Lipophilic | 8.2% | Use ≤20 mg/day |
| Pravastatin | Hydrophilic | 1.3% | Safe at standard doses |
| Rosuvastatin | Hydrophilic | 1.4% | Preferred first-line |
Simvastatin at 40 mg or higher is especially dangerous. The 2022 American College of Cardiology guidelines say it should be avoided entirely in hypothyroid patients. Rosuvastatin at 10-20 mg is now the top recommendation. It’s just as effective at lowering cholesterol but far safer for your muscles.
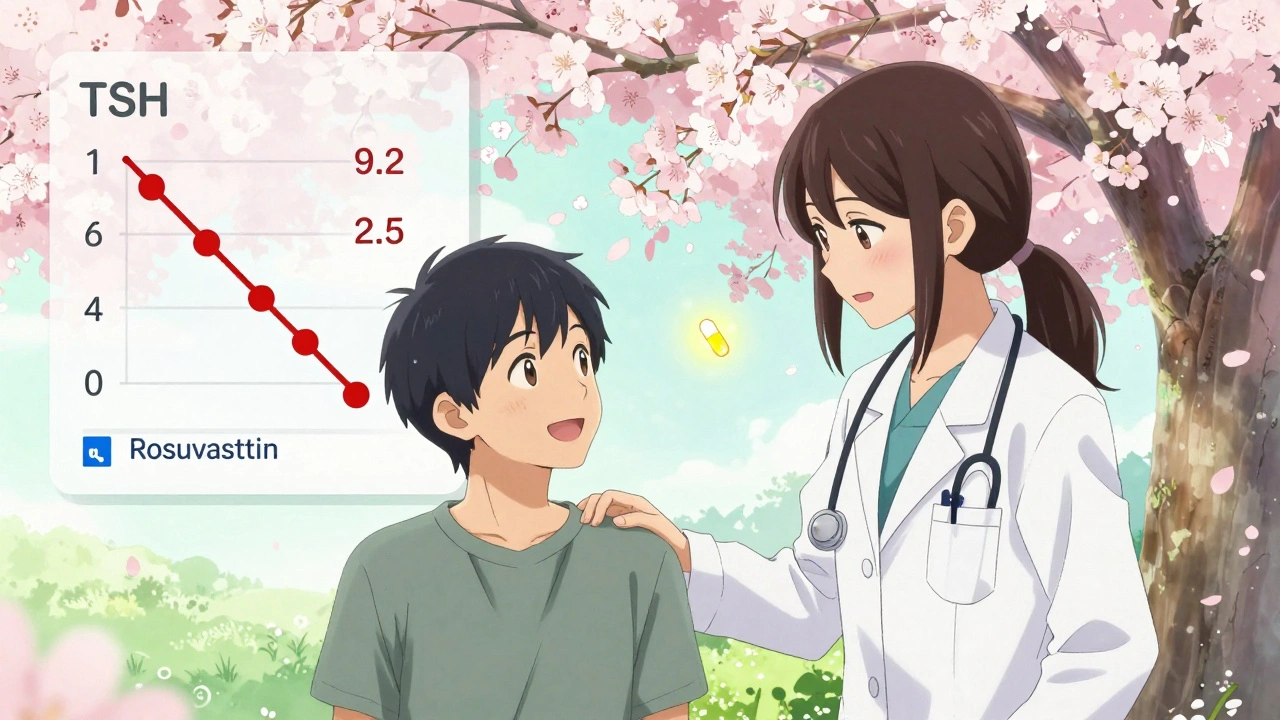
TSH - thyroid-stimulating hormone - is your thyroid’s warning light. Normal TSH is usually between 0.4 and 4.0 mIU/L. But for people on statins, that upper limit needs to be tighter.
Experts now recommend keeping TSH below 4.0 mIU/L, ideally between 0.5 and 3.0, before starting or continuing statins. Why? Because when TSH climbs above 4.0, your risk of muscle damage starts rising. At TSH levels above 7.0, the risk-benefit of statins becomes questionable. One cardiologist put it bluntly: “Don’t start a statin if your TSH is above 7.0. Fix the thyroid first.”
Even if you’re on levothyroxine, your dose might not be right. Many patients feel fine - no fatigue, no weight gain - but their TSH is still creeping up. That’s enough to make statins dangerous. Regular blood tests aren’t optional. They’re essential.
On health forums like Reddit and PatientsLikeMe, hypothyroid patients are sharing their experiences. One user, ‘HypoWarrior2022’, described his CK levels spiking to 8,400 U/L after starting atorvastatin while his TSH was 9.2. He had to stop all meds for three weeks. His symptoms vanished only after his levothyroxine dose was adjusted.
A 2023 survey of 1,245 hypothyroid statin users found that 73% who developed muscle pain had TSH levels above 4.5. When their thyroid levels were corrected, 89% saw their muscle pain go away within 4 to 6 weeks.
But the worst cases are tragic. A 67-year-old woman developed rhabdomyolysis with CK levels of 28,500 U/L while on simvastatin and preparing for radioactive iodine treatment. Her TSH was 22.4. She needed dialysis. This isn’t rare. It’s predictable.
Before starting any statin, your doctor should check your TSH and free T4. If you’re already on levothyroxine, get tested again 6-8 weeks after starting the statin or changing the dose. Don’t wait for muscle pain to show up.
Here’s what you can ask:
Some doctors still think, “It’s just muscle soreness - take it easy.” But in hypothyroid patients, even mild pain can be a sign of something serious. Don’t brush it off.
Some studies show that taking 200 mg of CoQ10 daily reduces muscle pain in hypothyroid statin users by over 50%. It’s not officially recommended in most guidelines, but it’s low-risk and biologically plausible. Since both hypothyroidism and statins lower CoQ10, replacing it makes sense.
It’s not a magic fix, but for people struggling with muscle pain despite optimized thyroid levels, it’s worth trying. Talk to your doctor about it. Don’t self-prescribe high doses without supervision.
Over 20 million Americans have hypothyroidism. Nearly 40 million take statins. Millions of them overlap. Yet, most people don’t know about this interaction. That’s why 32% of hypothyroid patients quit statins within a year - not because they don’t need them, but because they got muscle pain and no one told them to check their thyroid.
That’s a huge problem. Statins prevent heart attacks and strokes. Stopping them unnecessarily puts people at risk. The good news? When thyroid levels are optimized, 85-90% of hypothyroid patients can safely stay on statins. Their heart risk drops to match that of people with normal thyroid function.
Recent FDA and EMA guidelines are starting to catch up. New statin labels will soon include warnings about hypothyroidism. Clinical tools are being developed to predict risk based on genetics and thyroid status. But right now, the best tool is simple: check TSH. Adjust levothyroxine. Pick the right statin.
If you’re on statins and have hypothyroidism:
If you’re not on statins but have hypothyroidism and high cholesterol:
This isn’t about avoiding statins. It’s about using them safely. Your thyroid isn’t just a gland - it’s a gatekeeper for how your body handles medication. Treat it like one.
Yes. Many people with hypothyroidism don’t feel tired or gain weight - but their TSH is still elevated. Even mild thyroid dysfunction slows down how your liver breaks down statins, leading to higher drug levels in your blood. Muscle pain can appear without other symptoms. That’s why blood tests matter more than how you feel.
No - unless your TSH is very high (above 10) and you’re on a high-risk statin like simvastatin. Most people can safely stay on statins if their thyroid levels are optimized. Stopping statins unnecessarily increases your risk of heart attack or stroke. The goal is to fix the thyroid, not quit the statin.
Yes. Rosuvastatin is hydrophilic, meaning it doesn’t enter muscle cells as easily as lipophilic statins like simvastatin or atorvastatin. Studies show it causes 2-3 times less muscle damage in hypothyroid patients. It’s also less dependent on liver enzymes that are slowed by low thyroid function. For this group, it’s the safest first-choice statin.
Get tested before starting the statin, then again at 6-8 weeks after starting or changing the dose. After that, check every 6-12 months - or sooner if you develop muscle pain, fatigue, or unexplained weakness. Thyroid function can change over time, especially with age or other medications.
Evidence suggests yes. A 2020 trial showed 200 mg of CoQ10 daily reduced muscle pain by over 50% in hypothyroid patients on statins. It’s not a cure-all, but since both hypothyroidism and statins lower CoQ10, supplementing makes biological sense. Talk to your doctor before starting - it’s safe, but you still need to optimize your thyroid first.
Don’t ignore it. Call your doctor right away. Get a CK blood test. If your CK is more than 5 times the upper limit of normal - or more than 10 times even without symptoms - your statin should be stopped. But don’t assume it’s the statin’s fault. Your TSH might be too high. Fix the thyroid, then decide if you can restart a safer statin.
sean whitfield
5 12 25 / 15:34 PMSo basically the medical industrial complex wants you to take a drug that kills your muscles while ignoring the real problem: your thyroid is a canary in the coal mine and they'd rather sell you more pills than fix the root cause. CoQ10? Nah. Just stop the statin and eat some eggs.
Carole Nkosi
6 12 25 / 20:42 PMThis is why I stopped trusting doctors. They treat symptoms like they're puzzles to solve with chemicals instead of listening to the body. Hypothyroidism isn't a footnote in a statin pamphlet-it's the main character. Fix the thyroid or don't touch the statin. Simple.
Stephanie Bodde
7 12 25 / 02:30 AMYou're not alone!! 🙌 I was on simvastatin and felt like a zombie with muscle pain-turned out my TSH was 8.5. After switching to rosuvastatin and tweaking my levothyroxine, I'm back to hiking and yoga! 💪甲状腺是关键!❤️
Philip Kristy Wijaya
8 12 25 / 22:19 PMThe data presented here is statistically significant and clinically relevant however one must consider the confounding variables such as genetic polymorphisms in SLCO1B1 and CYP3A4 which may independently influence statin pharmacokinetics the assertion that TSH alone dictates risk is reductive and potentially dangerous in clinical practice
Jennifer Patrician
10 12 25 / 13:18 PMThey don't want you to know this. Big Pharma and endocrinology are in bed together. Why? Because if you fix your thyroid first, you don't need their expensive statins. They'll keep pushing simvastatin until you're in the ER with rhabdo. TSH above 4? That's not a lab result-it's a red flag. Wake up.
Manish Shankar
10 12 25 / 18:53 PMThank you for this comprehensive and clinically grounded analysis. As a physician, I have observed this interaction repeatedly in practice. The most critical intervention remains the optimization of thyroid function prior to statin initiation. The data on hydrophilic statins is robust and should guide clinical decision-making.
Rupa DasGupta
12 12 25 / 05:30 AMI cried reading this. My TSH was 11.2 when I started atorvastatin. I thought I was just getting old. My legs gave out. I couldn't climb stairs. My doctor said "it's just muscle soreness". I lost 3 months of my life. Now I'm on rosuvastatin 10mg and my TSH is 2.1. I'm alive again. CoQ10 helped too. Don't wait like I did. 🥺
Marvin Gordon
12 12 25 / 16:10 PMThis is the kind of info that saves lives. Seriously. If you're on statins and have hypothyroidism, this isn't optional reading-it's survival prep. Get your TSH checked. Switch statins if needed. Talk to your doc. Your muscles will thank you.