
Switching from a generic medication back to the brand-name version isn’t as simple as asking your pharmacist for the original. It’s a medical decision, not a preference. Many people assume generics are just cheaper versions of the same thing-and for most, they are. But for some, even tiny differences in inactive ingredients can cause real problems. If you’ve noticed new side effects, worsening symptoms, or strange reactions after switching to a generic, you’re not imagining it. And you’re not alone. Thousands of patients report similar issues every year. The question isn’t whether you can switch back-it’s whether you should, and how to do it without risking your health or getting stuck in insurance red tape.
Why Switching Back Might Be Necessary
Generic drugs are required by the FDA to contain the same active ingredient, strength, and dosage form as the brand-name version. That part is non-negotiable. But here’s what’s often overlooked: the fillers, dyes, binders, and coatings can be completely different. These inactive ingredients don’t treat your condition, but they can trigger reactions in sensitive people. A patient with a peanut allergy might react to a generic version that uses peanut oil as a binder. Someone with celiac disease might get sick from a generic that uses wheat starch. Others report rashes, headaches, nausea, or even a return of symptoms like seizures or unstable blood thinning after switching to a generic.
For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or certain epilepsy meds-small changes in absorption can be dangerous. The FDA allows generics to vary by up to 20% in how much of the drug enters your bloodstream compared to the brand. That’s fine for most medications. But for warfarin, a 10% change can mean the difference between a clot and a stroke. In these cases, consistency matters more than cost.
When Switching Back Is Medically Supported
Doctors don’t switch patients back to brand-name drugs lightly. But there are clear clinical reasons they will. The American College of Clinical Pharmacy says switching back is justified when:
- Therapeutic failure occurs-your condition worsens after switching to generic
- You develop new or worsening side effects linked to inactive ingredients
- You’re taking a narrow therapeutic index drug and lab results show instability
- You’ve had a documented allergic reaction to a specific filler in the generic
For example, a patient on levothyroxine who switches to a generic and then sees their TSH levels jump from 2.1 to 8.7 over two months isn’t just being picky. That’s a clinical red flag. Same with someone on phenytoin who starts having breakthrough seizures after a generic switch. These aren’t anecdotes-they’re documented patterns in FDA adverse event reports and peer-reviewed studies.
How to Start the Process
You can’t just walk into a pharmacy and ask for the brand. Pharmacists are legally required to dispense the cheapest option unless the doctor says otherwise. So the first step isn’t calling your pharmacy-it’s talking to your doctor.
Step 1: Document your experience
Write down exactly what changed after you switched. When did symptoms start? What were they? Did your blood pressure, INR, thyroid levels, or seizure frequency change? Bring lab results if you have them. Don’t say, “I feel worse.” Say, “My INR jumped from 2.5 to 4.1 two weeks after switching to generic warfarin.” Specificity saves time and builds your case.
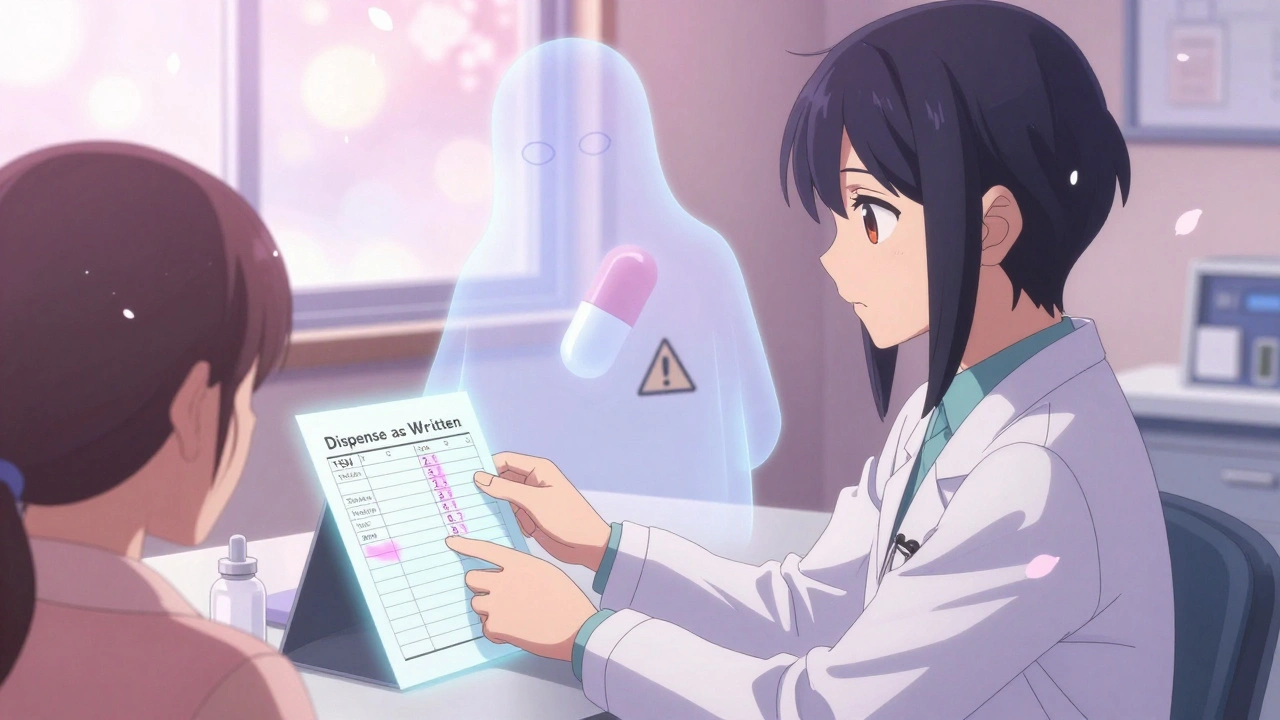
Step 2: Ask your doctor to write a ‘Brand Medically Necessary’ prescription
Your doctor needs to write “Dispense as Written” or “Brand Medically Necessary” on the prescription. Some EHR systems have a checkbox for this. If yours doesn’t, they can write it by hand. For Medicare Part D, this triggers a special exception process. Without this note, your insurance will deny the claim every time.
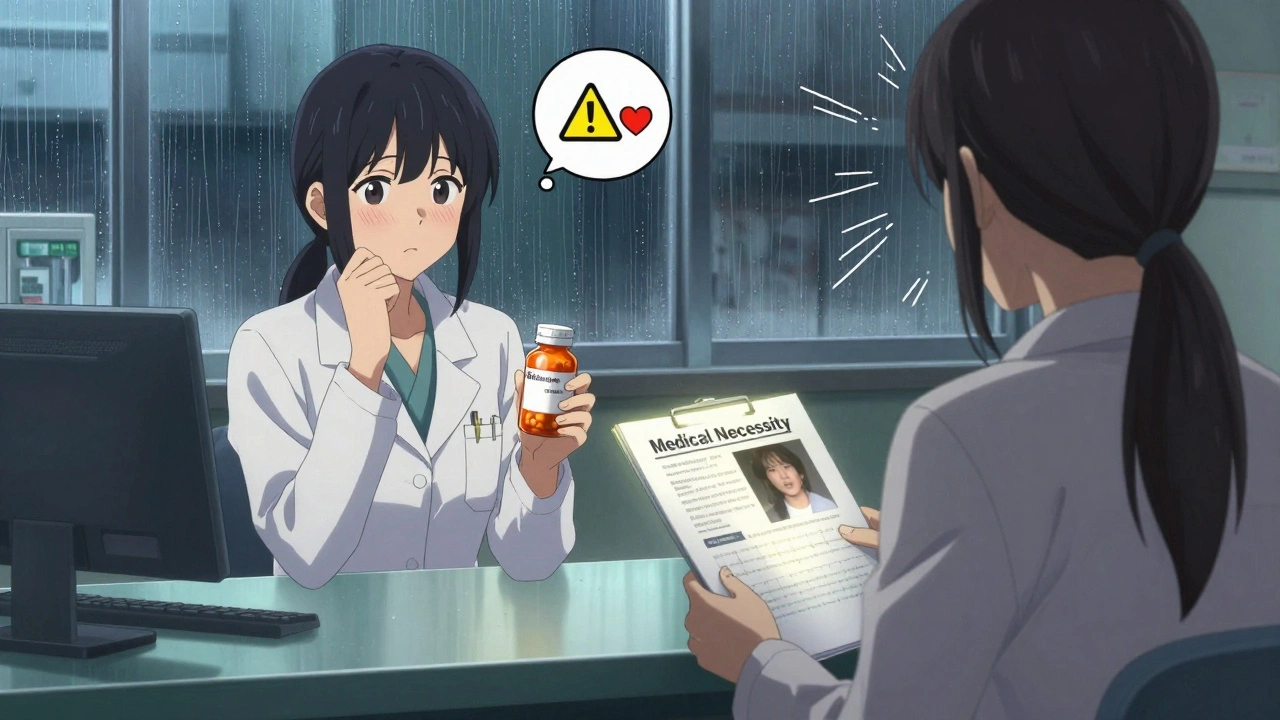
Step 3: Include clinical evidence
The more proof you have, the better. A 2022 JAMA study found that 63.7% of denied brand-name requests were approved on appeal-
if the doctor included lab data, dosage history, and clear clinical justification. Attach recent blood work, symptom logs, or even a letter from your specialist. For thyroid patients, a TSH and free T4 from before and after the switch makes a powerful case.
What Happens After the Prescription Is Written
Even with the right paperwork, you might hit roadblocks. Insurance companies hate paying more for brand-name drugs. Medicare Part D plans require prior authorization for 68% of brand-name drugs when a generic exists. That means your doctor’s office has to submit paperwork, and you might wait up to two weeks.
Here’s what to do:
- Call your insurance company and ask for the prior authorization form number
- Ask your doctor’s office to submit it immediately
- Keep a copy of everything-prescription, lab results, denial letters
If you get denied, don’t give up. Most denials can be appealed. The key is persistence. In one case, a patient with epilepsy was denied brand-name lamotrigine three times. Each time, their neurologist added more data: seizure frequency logs, EEG results, and a letter citing the 2022 AAN guideline that warned against switching in epilepsy patients. On the fourth try, it was approved.
What to Expect at the Pharmacy
Even with a valid prescription, some pharmacists may hesitate. A 2022 SurveyMonkey poll found 41.7% of patients who requested brand-name drugs were initially refused-often because the pharmacist didn’t recognize the “Brand Medically Necessary” note.
If this happens:
- Ask to speak to the pharmacist on duty
- Have your doctor’s phone number handy
- Politely remind them that federal law (CMS guidelines) requires them to fill a prescription marked “Dispense as Written”
Some pharmacies have policies that require them to call the prescriber to confirm. That’s normal. Don’t get angry-just stay calm and provide the contact info. Most issues get resolved within an hour.
Costs and Insurance Realities
Brand-name drugs cost 3 to 5 times more than generics. A monthly supply of Synthroid might be $110 as a generic, but $450 as the brand. That’s a huge difference. But here’s the catch: many insurance plans have a tiered system. If your doctor proves medical necessity, your plan might cover it at the same cost as a generic.
Some patients get lucky. One woman on Reddit reported her insurance covered Synthroid immediately after her endocrinologist wrote “medically necessary.” But that’s not the norm. More often, you’ll need to go through prior authorization, appeals, or even pay out-of-pocket for a few weeks.
There are options:
- Ask your doctor about manufacturer coupons or patient assistance programs
- Check GoodRx or SingleCare for cash prices-sometimes the brand is cheaper than your insurance copay
- Ask if the brand company sells an “authorized generic”-same formula, lower price
When You Shouldn’t Switch Back
Not every complaint about a generic is a medical emergency. The American Medical Association warns that 99.7% of generic switches are perfectly safe. Many patients report feeling “different” after switching, but their labs show no change. In those cases, switching back doesn’t help-and it costs the system more money.
Avoid switching back if:
- Your symptoms started before you switched to the generic
- You’re taking a medication with a wide therapeutic index (like most antibiotics or statins)
- You’re switching between two different generics (not brand to generic)
- Your doctor says your lab results are stable
Switching back just because “I like the brand better” isn’t a valid medical reason. But if your body reacts differently? That’s different.
Long-Term Considerations
Once you’re back on the brand, stay there. Don’t let your doctor or pharmacist switch you again without your consent. Ask them to note in your chart: “Do not substitute. Brand medically necessary.” This protects you from future changes.
Also, keep an eye on your medication. Brand manufacturers rarely change their formulas. Generics? Not so much. A generic made by Company A might be fine, but if your pharmacy switches to Company B, you could be back to square one. Always check the name on the bottle.
What’s Changing in 2025
The FDA is pushing for better labeling of inactive ingredients on generic packaging. Starting in 2025, all generic drugs must list all fillers on the label-something that’s currently optional. That’s a big win for patients who need to avoid certain substances.
Medicare Part D is also rolling out a new “Medically Necessary Brand Exception” pathway in 2025. It guarantees a decision within 72 hours for certain high-risk drugs like warfarin, levothyroxine, and anti-seizure meds. That’s faster than the current 14-day average.
Final Thoughts
Switching back from a generic to a brand isn’t about privilege-it’s about safety. If your body tells you something’s wrong, listen. But don’t act alone. Work with your doctor. Document everything. Know your rights. Insurance will fight you, but with the right paperwork, you can win. You’re not asking for luxury. You’re asking for stability. And that’s not too much to ask.
Can I switch back to a brand-name drug just because I prefer it?
No. Insurance companies and pharmacies require a documented medical reason to cover a brand-name drug when a generic exists. Preference alone won’t qualify you. You need evidence of therapeutic failure, side effects, or instability tied to the generic version.
How long does it take to get insurance approval to switch back?
It can take anywhere from a few days to three weeks. Medicare Part D currently averages 14.3 days for prior authorization. But under the new 2025 rules, certain high-risk drugs will get decisions within 72 hours. Always follow up with your doctor’s office and insurance if it’s been over a week.
Are all generics the same?
No. While all generics must meet FDA bioequivalence standards, different manufacturers use different inactive ingredients. One generic might use cornstarch, another might use lactose or dye. If you’ve had a reaction to one generic, switching to another might not help. Always check the manufacturer name on the bottle.
Which medications are most risky to switch between?
Drugs with a narrow therapeutic index are the most dangerous to switch. These include warfarin, levothyroxine, phenytoin, carbamazepine, lithium, and cyclosporine. Even small changes in absorption can lead to serious harm. The FDA specifically warns against switching between brands and generics for these drugs without close monitoring.
What if my pharmacy refuses to fill my brand-name prescription?
If your prescription clearly says “Dispense as Written” or “Brand Medically Necessary,” the pharmacy is legally required to fill it. If they refuse, ask to speak to the pharmacist on duty and show them the note. If they still refuse, call your doctor’s office-they can call the pharmacy directly. You can also file a complaint with your state board of pharmacy.
Can I switch back to the brand if I’ve already tried multiple generics?
Yes. If you’ve tried two or more different generic versions and still have issues, that strengthens your case. Document each switch and how you reacted. This pattern shows the problem isn’t one specific generic-it’s likely the class of generics as a whole, making your request for the brand more credible.

Casey Mellish
13 12 25 / 19:37 PMAs an Aussie with a thyroid condition, I’ve been through this exact battle. Switched to generic levothyroxine, woke up feeling like a zombie for six weeks. TSH went from 1.8 to 7.3. My endo didn’t believe me until I showed the lab results. Took three appeals, but we got the brand back. Now I’m stable. Don’t let anyone tell you it’s ‘all in your head.’ Your body knows.
Also, check if your pharmacy switched manufacturers. I got hit twice-first by one generic, then another-same pill, different filler. Always look at the manufacturer name on the bottle. It’s not the drug, it’s the junk they put around it.
Tommy Watson
15 12 25 / 11:21 AMbro why are we even paying for brand names?? like i get it if u have seizures or sumthin but most people just wanna whine bc they think brand = better. generic is the same damn thing. save your cash and stop being a medical drama queen.
Rawlson King
16 12 25 / 22:15 PMThere is no such thing as ‘brand medically necessary’ unless it’s backed by peer-reviewed clinical evidence. The FDA’s bioequivalence standards are robust. If a patient experiences adverse effects, it’s more likely psychosomatic or due to non-adherence than the inactive ingredients. The pharmaceutical industry has spent decades marketing fear to drive profits. Don’t be manipulated.
Lara Tobin
18 12 25 / 19:19 PMI just want to say thank you for writing this. I’ve been too scared to speak up because everyone says I’m being dramatic. I switched to a generic warfarin and my INR went from 2.6 to 4.9. I nearly bled out. My doctor didn’t take me seriously until I brought the lab results. Now I’m back on Synthroid and I sleep at night again. You’re not alone. And you’re not crazy.
❤️
Jamie Clark
19 12 25 / 08:38 AMThis whole ‘I feel different’ nonsense is why American healthcare is broken. You’re not special because your body reacts to cornstarch. There are millions of people taking generics without issue. You want the brand? Pay for it yourself. Stop making insurers and doctors jump through hoops for your emotional whim. The system isn’t designed to coddle your placebo-driven paranoia.
Keasha Trawick
20 12 25 / 09:40 AMLet’s get real: generics are bioequivalent, sure-but ‘equivalent’ doesn’t mean ‘identical.’ We’re talking about excipients: dyes, lactose, gluten, talc, even peanut oil in some obscure formulations. For someone with a rare allergy or autoimmune sensitivity, this isn’t a ‘preference,’ it’s a life-or-death variable.
And let’s not forget the 2022 JAMA meta-analysis showing 63.7% of denied brand requests were approved on appeal-*with documentation*. This isn’t about privilege. It’s about pharmacogenomics. We’re not all the same chemical reactor. Some of us are finely tuned instruments, and generics? They’re tuning forks with mismatched frequencies.
Also, the 20% bioavailability variance? That’s a 10% swing in warfarin. That’s not ‘fine.’ That’s a stroke waiting to happen. The FDA’s standards are a minimum, not a guarantee.
Bruno Janssen
20 12 25 / 23:41 PMI used to work in pharmacy. I saw it all. People crying because their generic pill was a different color. Some of them were right. Some were just scared. But the ones who had real reactions? They didn’t complain. They showed up with labs, logs, doctor notes. And we filled it. The system’s broken, but the patients who fight smart? They win.
I just wish more people knew how to fight smart.
Emma Sbarge
21 12 25 / 21:36 PMWhy are we letting corporations decide what’s safe for our bodies? The FDA lets generics vary by 20%? That’s insane. You wouldn’t let a mechanic use ‘close enough’ parts on your brakes. Why are we okay with this for our brain, heart, thyroid? This isn’t about being picky. It’s about corporate greed hiding behind ‘cost savings.’
And don’t get me started on how pharmacies switch manufacturers without telling you. You think you’re on the same generic? You’re not. It’s like buying the same car model but getting a different engine every time.
Deborah Andrich
22 12 25 / 06:14 AMThank you for this. I’ve been silent for years. I had seizures after switching to a generic phenytoin. My neurologist said it was stress. I brought my EEGs. I brought my logs. I brought the FDA’s own warning about narrow therapeutic index drugs. They finally listened.
To anyone reading this: don’t let anyone make you feel crazy for needing stability. Your health isn’t a budget line item. And if your doctor won’t help, find one who will.
You’re not alone. We’re here.
Donna Hammond
22 12 25 / 08:10 AMI’m a pharmacist in Ohio. I’ve filled thousands of generics. I’ve also filled dozens of ‘Brand Medically Necessary’ scripts. Here’s the truth: 90% of patients who ask for the brand are fine on generics. But the other 10%? They’re the ones who would die without it. Warfarin. Levothyroxine. Phenytoin. These aren’t placebos. These are precision tools.
My advice? Document everything. Lab results. Symptom timelines. Manufacturer names. Bring it to your doctor. Don’t argue with the pharmacy. Have your doctor call them. Most issues get solved in 15 minutes.
And yes, if you’ve tried three generics and still react? You’re not weird. You’re a data point. And data matters.
Willie Onst
23 12 25 / 07:37 AMJust want to say this post saved my life. I was about to quit my meds because I felt like I was losing my mind. Turns out, it was the generic. Now I’m back on brand, and I’m actually sleeping again. Thanks for the roadmap. You’re a real one.