
Drug Safety Checker
Enter your medications to check for safety warnings and potential interactions. This tool helps identify critical information from prescription drug labels.
Every time you pick up a prescription, there’s a hidden guide inside that could save your life. It’s not the pill bottle, or the receipt, or even the pharmacist’s quick advice. It’s the safety and warnings section on the drug label - a detailed, legally required breakdown of what could go wrong, what to watch for, and how to avoid serious harm. Most people glance at it, maybe read the big red warning sticker, and move on. But if you really understand what’s written there, you can prevent hospital visits, dangerous interactions, and even death.
What the Boxed Warning Really Means
The most serious warning on any prescription label is the
boxed warning, also called a
black box warning. It’s called that because it’s printed in a thick black border, like a warning sign on a construction site. This isn’t just a suggestion. The FDA requires this format for drugs that carry a risk of death or life-threatening side effects. If you see this, you’re looking at the highest level of danger.
For example, clozapine, used for severe schizophrenia, has a boxed warning because it can destroy white blood cells - a condition called agranulocytosis. Without regular blood tests, this can kill you. Another example is fluoroquinolone antibiotics like ciprofloxacin - they can cause tendon rupture, even in healthy people. These aren’t rare. The FDA tracks over 400 medications with boxed warnings as of 2023.
Don’t ignore this. If your drug has a black box, ask your doctor:
“What are the signs I need to watch for?” and
“How often do I need tests?” Don’t assume the pharmacist told you everything. Many patients don’t even know what the box means. A 2021 study found 68% of patients didn’t recognize the term “black box” as a serious warning.
Warnings and Precautions: The Fine Print That Matters
Right after the boxed warning comes the “Warnings and Precautions” section. This is where the real details live. It’s not just a list of side effects. It’s a list of risks that have actually happened in real patients - not just theoretical possibilities.
Look for phrases like:
- “May cause dizziness or fainting” - this means it’s common enough to be dangerous during daily activities.
- “Has been associated with liver injury” - this means real cases have been reported, not just lab results.
- “Use with caution in patients with kidney disease” - this tells you if your existing condition changes the risk.
These aren’t random. The FDA requires drug makers to use specific language. If it says “may cause,” it’s based on clinical trial data. If it says “has been reported,” it’s from post-market reports - meaning real people had the problem after taking the drug.
Pay special attention to warnings about
timing. For example: “Take on an empty stomach” or “Avoid alcohol for 48 hours.” These aren’t suggestions. Taking a drug with food when it says not to can make it useless - or dangerously strong. One patient in 2022 ended up in the ER after taking dextromethorphan with an SSRI antidepressant, ignoring the “do not take with SSRIs” warning. He developed serotonin syndrome - a potentially fatal reaction.
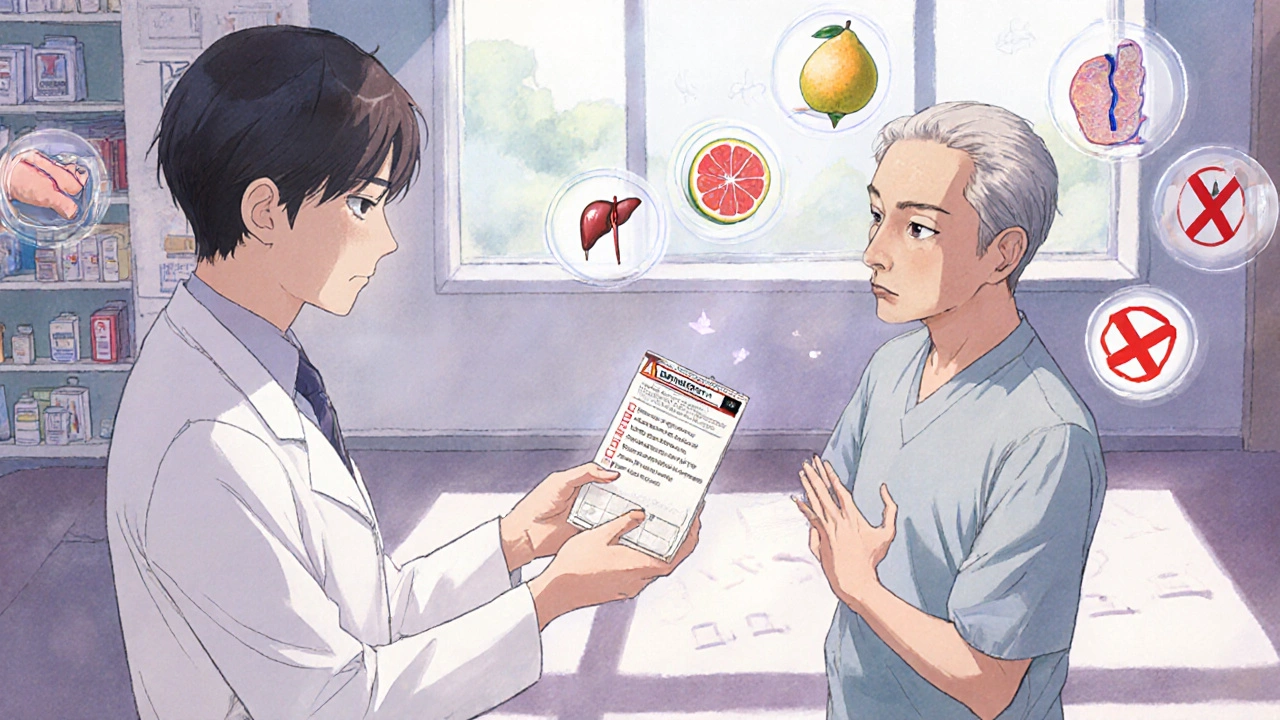
Drug Interactions: When Your Other Meds Turn Dangerous
This is where most people get caught off guard. You’re taking your blood pressure pill, your painkiller, your vitamin, and your new antibiotic. What happens when they all mix?
The “Drug Interactions” section doesn’t just say “may interact.” It tells you
how. For example:
- “CYP3A4 inhibitors may increase plasma concentrations of this drug by up to 400%” - that’s not jargon. It means if you take this with grapefruit juice, certain antibiotics, or even some heart medications, your drug level could spike to four times the safe amount.
- “May reduce effectiveness of birth control pills” - this is a real risk with some antibiotics and seizure meds. You need backup contraception.
A 2023 Reddit survey of over 1,200 patients found that 73% were confused about interactions, especially when taking five or more medications. That’s not surprising - pharmacists often have to abbreviate warnings to fit on small bottles. A child’s medicine vial has 75% less space than an adult’s.
Solution? Keep a simple list of everything you take - including supplements and over-the-counter drugs. Bring it to every appointment. Ask: “Could any of these react with my new prescription?”
What the Pharmacy Label Tells You (And What It Leaves Out)
The sticker on your bottle - the one with big letters - is the pharmacy’s version of the warning. It’s meant to be clear, quick, and easy to read. But it’s not complete.
You’ll see things like:
- “May cause drowsiness - do not drive”
- “Take 2 hours before meals”
- “Avoid alcohol”
These are critical. But they’re also simplified. The full warning might say “May cause sedation and impaired psychomotor performance, increasing risk of falls in elderly patients.” The pharmacy sticker cuts that down to “May cause drowsiness.”
Here’s the problem: 38% of patients report that critical warnings are printed on the bottom of the bottle - where they get hidden when stored in a medicine cabinet. If you can’t see it, you can’t follow it.
Tip: When you get your prescription, read the sticker. Then ask the pharmacist: “Is there anything else I should know that’s not on this label?” They’re trained to catch the hidden risks.
Why Health Literacy Changes Everything
It’s not just about reading the words. It’s about understanding them. A 2012 study found patients with low health literacy were 3.2 times more likely to misunderstand warnings - especially ones with numbers.
Examples:
- “Take 1 tablet every 6 hours, not to exceed 4 doses in 24 hours” - many people think “every 6 hours” means four times a day, but they don’t realize it’s a 24-hour limit. Taking one extra dose can cause liver damage from acetaminophen.
- “Use only as directed” - this sounds vague, but it’s a legal term meaning: don’t take more, don’t take longer, don’t give to others.
The FDA’s own data shows that 52% of patients misunderstand timing instructions, and 41% miss interaction warnings when juggling multiple drugs.
The fix? The “teach-back” method. After the pharmacist explains a warning, say: “So, just to make sure I got it - you’re saying I need to avoid grapefruit because it can make this drug too strong, right?” If you can say it back in your own words, you’ve understood it.
Studies show this reduces medication errors by 27% in older adults.
What’s Changing - and What You Should Watch For
The system is evolving. In 2024, the FDA started requiring new drugs to test their warning language with real patients - especially those with low reading skills. That means future labels will be simpler, clearer, and less full of medical jargon.
New tech is coming too. Some pharmacies are testing NFC chips on bottles. Tap your phone on the label, and a short video explains the warning in plain language. In pilot programs, comprehension jumped from 63% to 92%.
But not everyone has a smartphone. That’s why analog solutions still matter. The American Pharmacists Association recommends creating a personal “warning log” - a small card or note that lists your meds and their top risks. One University of Florida study found this improved adherence to safety rules by 41% in seniors.
What to Do Next - A Simple Action Plan
You don’t need to be a doctor to read these labels. You just need to be curious. Here’s what to do every time you get a new prescription:
- Find the boxed warning. If it’s there, don’t skip it. Ask your doctor what signs to watch for and how often you need tests.
- Read the pharmacy sticker. If it’s hard to see, ask for a larger copy or a printed sheet.
- Check for timing and food warnings. “Take on empty stomach” isn’t optional. “Avoid alcohol” isn’t a suggestion.
- List all your meds. Include vitamins, herbs, and OTC drugs. Bring this to every appointment.
- Use the teach-back method. Say back what you heard in your own words. If you’re unsure, say: “Can you explain that again?”
- Consider a warning log. Write down your top 3 risks for each drug. Keep it in your wallet or phone notes.
Final Thought: This Isn’t Just About Reading - It’s About Understanding
Prescription labels aren’t designed to scare you. They’re designed to protect you. The warnings aren’t there because drugs are dangerous - they’re there because people can be careless. A single misunderstood warning can lead to an emergency room visit, a hospital stay, or worse.
You don’t need to memorize every detail. But you do need to know the big ones. If you take one thing from this, let it be this:
Never assume you understand a warning. Always ask until you do. Your life might depend on it.

Erin Nemo
29 11 25 / 21:35 PMJust read my new blood pressure pill label and saw 'avoid grapefruit' - had no idea it could mess with the dose. Thanks for the heads-up.
Suzanne Mollaneda Padin
30 11 25 / 11:35 AMI work in a pharmacy and see this every day. Patients often miss the timing stuff - like taking meds with food when it says 'empty stomach.' It’s not just about side effects, it’s about efficacy. A pill that doesn’t work because of food is just as dangerous as one that causes harm.
Always ask: 'Is this going to work the way it’s supposed to?' Not just 'Will it hurt me?'
Also, keep a physical list. Digital apps fail. Phones die. Batteries drain. A folded piece of paper in your wallet? Still works in 2024.
Bonnie Youn
1 12 25 / 03:54 AMOMG YES this is so important I can’t believe people ignore this stuff
My aunt took that antibiotic with her grapefruit juice and ended up in the ICU for a week
She didn’t even know grapefruit was a thing
Don’t be like her
Read the tiny print
Your body will thank you
Also tell your grandma
Kenny Leow
2 12 25 / 00:59 AMAs someone who grew up in a household where meds were just 'take it when it hurts,' this post changed how I think about prescriptions.
It’s not about fear - it’s about respect.
The label isn’t bureaucracy. It’s a bridge between science and survival.
And yes, the black box? That’s not a warning. That’s a lifeline.
Thanks for writing this with clarity. We need more of it.
James Allen
3 12 25 / 16:29 PMLook, I get it - the FDA wants us to read labels. But let’s be real. Most people are working two jobs, raising kids, and trying not to lose their minds. You think they’re sitting down with a magnifying glass to parse 'CYP3A4 inhibitors'?
Meanwhile, Big Pharma is making billions off the confusion.
This isn’t education - it’s a liability shield wrapped in legalese.
Fix the system. Don’t blame the patient.
Rachel Stanton
4 12 25 / 18:41 PMOne thing people overlook: the difference between 'may cause' and 'has been reported.' The former is clinical trial data - controlled, limited. The latter? Real-world chaos. Someone took it with whiskey, forgot their kidney disease, and ended up in dialysis.
That’s why post-market surveillance matters.
And if you’re on five meds? You’re basically a walking pharmacology experiment.
Keep a log. Write it down. Even if it’s just a sticky note on your mirror.
Also - teach-back is not optional. Say it out loud. If you stumble, you didn’t get it. Ask again.
Lauryn Smith
5 12 25 / 14:17 PMI’m 68 and started using a warning log after my last hospital visit. Wrote down my meds and the top 3 risks on a 3x5 card. Kept it in my wallet.
My pharmacist cried when she saw it. Said she’d never seen a patient do that.
It’s not hard. Just write it. One line per drug.
You don’t need to be smart. You just need to care enough to write it down.
Mary Ngo
7 12 25 / 10:59 AMLet’s be honest - this is all part of the surveillance state. The FDA doesn’t care if you live or die. They care about lawsuits. The black box? It’s not to protect you. It’s to protect the drug company from being sued when you drop dead.
And don’t get me started on NFC chips. They’re tracking your medication habits. Who’s accessing that data? Who owns it?
They want you to scan your pill bottle like a loyal consumer. It’s not safety. It’s control.
Read the label? Fine. But ask: who benefits from you reading it?
Edward Hyde
9 12 25 / 00:45 AMWow. This is the most boring thing I’ve read all week. Like, congrats, you turned a 30-second pharmacist warning into a 10-page essay. Did you really need to cite 5 studies to say 'don’t mix grapefruit with your meds'? I’m not a doctor but even I know that.
Also, 'teach-back method'? That’s not a thing. That’s a therapist’s buzzword.
Just don’t be an idiot. Take the pill. Don’t drink. Don’t mix. Done.
Alexander Williams
10 12 25 / 17:46 PMThe entire premise is flawed. You’re assuming patients have the cognitive bandwidth to parse pharmacokinetic interactions when the average American reads at a 7th-grade level. The problem isn’t literacy - it’s systemic design failure.
The label isn’t the solution. It’s the symptom.
What we need is mandatory AI-assisted patient risk profiling at the point of prescribing - integrating EHRs, polypharmacy algorithms, and real-time interaction scoring. The current model is analog in a digital age.
And yes - I’ve published on CYP450 dynamics in JAMA.