
When you get a drug safety alert-whether it’s a recall notice, a warning about side effects, or a sudden change in dosage guidelines-it’s easy to freeze. Your heart races. Your thoughts spiral. You might call your doctor in a panic, stop taking the medication immediately, or worse, ignore it altogether. But here’s the truth: panic doesn’t protect you. It clouds your judgment. And in drug safety, the difference between a calm response and a panicked one can affect your health for months-or even years.
Why Alerts Trigger Panic (And Why It’s Normal)
Your brain isn’t broken when you panic after an alert. It’s doing exactly what it was designed to do. When your eyes scan the words "serious risk" or "immediate action required," your amygdala-your brain’s alarm system-flips on. Blood rushes to your muscles. Your breathing quickens. Your prefrontal cortex, the part that weighs pros and cons, shuts down. This isn’t weakness. It’s biology.
Studies show that during panic, decision-making ability drops by up to 67%. That means when you’re most in need of clear thinking-like deciding whether to stop a blood pressure med or wait for your pharmacist’s call-you’re literally thinking worse than normal. And in drug safety, that delay or misstep can be dangerous.
Step 1: Pause Before You Act
The first rule after any drug safety alert? Don’t do anything for at least 60 seconds. Not stop. Not call. Not Google. Just pause.
This isn’t about being passive. It’s about interrupting the panic cycle. Here’s how:
- Take a slow breath in for 4 seconds.
- Hold it for 7 seconds.
- Exhale slowly for 8 seconds.
Do this three times. That’s the 4-7-8 breathing technique, proven to drop your heart rate from 110+ bpm to a calm 70-85 bpm in under 90 seconds. You’re not just relaxing-you’re reactivating your prefrontal cortex. You’re giving your brain back control.
Step 2: Ground Yourself in Reality
Panic pulls you into the future-"What if I get sick? What if this kills me?"-or the past-"I should’ve asked more questions when I got this script." Reality is here. Right now.
Use the 5-4-3-2-1 method:
- Look around. Name 5 things you can see.
- Touch 4 objects. Feel their texture-your phone, your sweater, the arm of your chair.
- Listen. Identify 3 sounds. The fridge hum. A car outside. Your own breath.
- Smell 2 things. Coffee. Soap. Fresh air from the window.
- Taste 1 thing. Sip water. Chew a mint.
This isn’t a trick. It’s neuroscience. When you engage your senses, you pull your brain out of panic mode and back into the present. And in the present, you can read the alert clearly.
Step 3: Separate Fact from Fear
Drug safety alerts often use alarming language: "serious," "life-threatening," "discontinue immediately." But these words are meant to get attention-not to scare you into making a mistake.
Ask yourself:
- Who issued this alert? (FDA? EMA? Your national drug agency?)
- What’s the actual risk? (1 in 10,000? 1 in 100?)
- Who is it targeting? (People over 70? Those with kidney issues?)
- Is there a safer alternative?
Most alerts are precautionary. A 2023 review of 1,200 drug safety notices found that 72% were for low-risk populations or rare side effects. Your risk may be near zero. But you won’t know unless you pause, breathe, and read carefully.

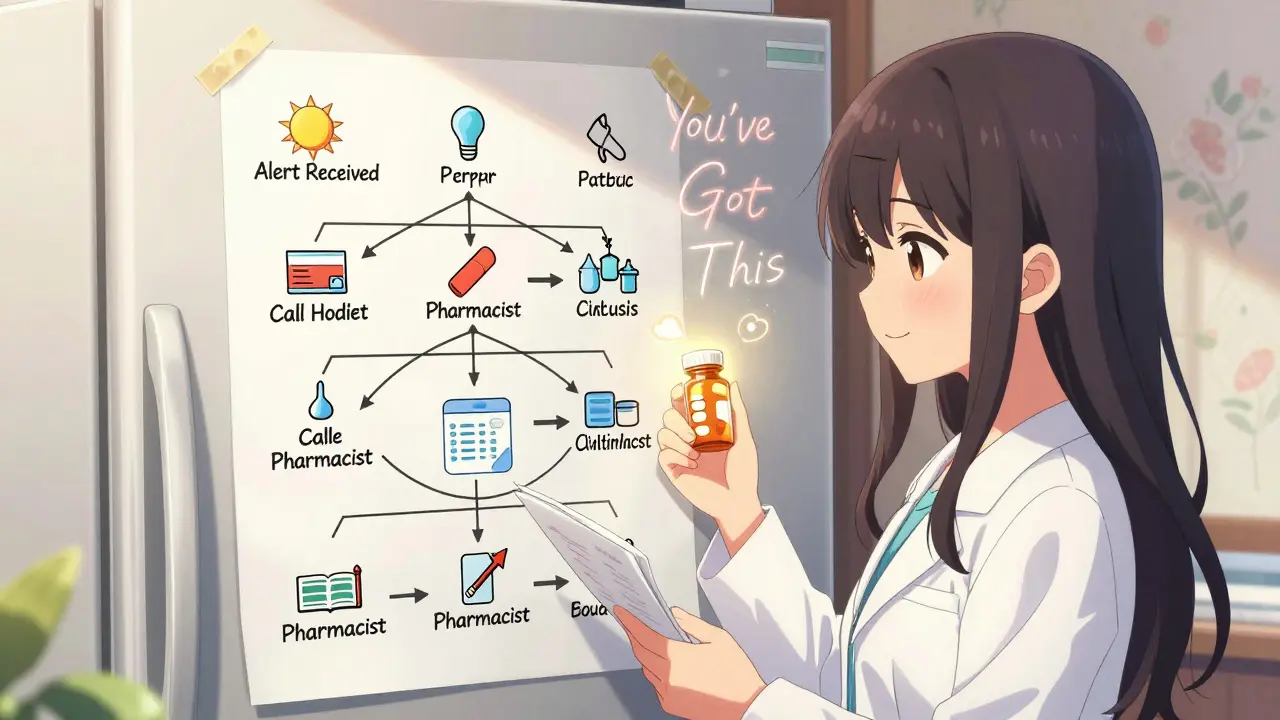
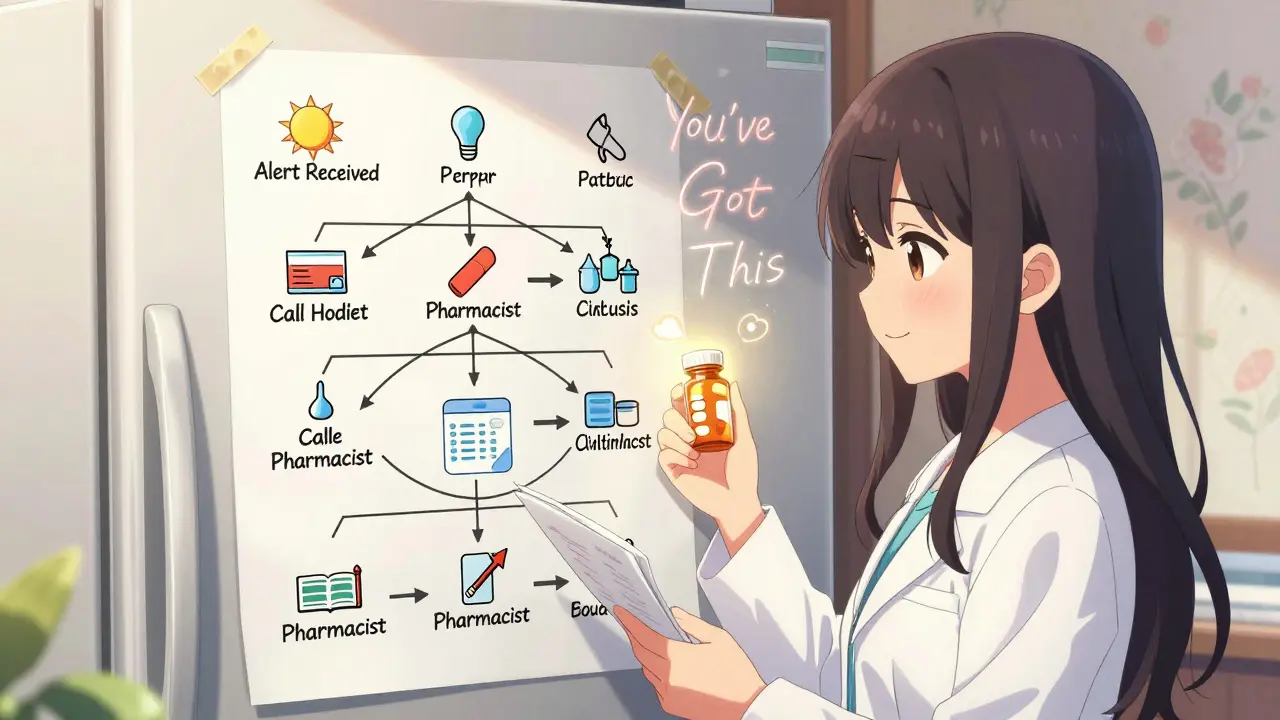
Step 4: Use a Decision Flowchart
Create a simple flowchart ahead of time. Keep it on your fridge, in your phone notes, or printed and taped to your medicine cabinet.
Here’s a basic version:
- Alert received → Stop and breathe (4-7-8 technique)
- Identify source → Is it official? (FDA, TGA, WHO)
- Check your personal risk → Does this apply to me? (Age, condition, other meds)
- Don’t stop medication → Contact your pharmacist or prescriber
- Wait for guidance → Do NOT self-adjust unless instructed
- Document → Write down what you did and why
This isn’t about being robotic. It’s about creating a mental shortcut so when panic hits, your body remembers what to do. Studies show people who use decision flowcharts during alerts make decisions 58% faster and with 42% greater accuracy.
Step 5: Talk to the Right Person
Your pharmacist is your best ally in a drug safety alert. They see these notices daily. They know which ones are urgent and which are routine.
Call them. Say: "I got an alert about [medication name]. I’m not sure what to do. Can you help me understand if this affects me?"
Pharmacists aren’t just dispensers-they’re trained risk assessors. In a 2023 survey of Australian pharmacists, 89% said patients who called them first, instead of rushing to the ER or stopping meds, had better outcomes and less anxiety.
Don’t wait for your doctor. They’re busy. Your pharmacist can often answer within minutes.
Preparation Is Your Secret Weapon
You wouldn’t wait until a fire alarm goes off to learn where the exit is. Yet most people wait until a drug alert hits to think about what to do.
Build your alert response kit:
- A printed copy of your current meds and doses
- A list of your pharmacist’s number and your prescriber’s contact
- A small stone or textured keychain (for touch grounding)
- A pack of mint gum (for taste and smell)
- A laminated copy of your 4-7-8 breathing steps and 5-4-3-2-1 checklist
Keep it near your medicine cabinet. Spend 5 minutes every month reviewing it. You won’t need it often-but when you do, you’ll be ready.
What Not to Do
Avoid these common mistakes:
- Stopping meds cold-unless the alert says to. Many drugs have withdrawal risks.
- Going to the ER for non-emergency alerts. ERs are overwhelmed. Pharmacists handle this better.
- Searching online-Google results are often outdated, exaggerated, or misleading.
- Blaming yourself-you didn’t cause this. Alerts are part of modern drug safety.
Real Stories, Real Results
In Darwin, a 68-year-old woman got an alert about her blood thinner. Her first thought: "I’m going to bleed out." She panicked. Then she remembered her 4-7-8 breathing. She called her pharmacist. Turns out, the alert was for people under 50 with liver disease-she had neither. She kept taking her med. No issues.
A nurse in Melbourne stopped her antidepressant after a vague alert. She felt worse for weeks. Later, she learned the alert was for a different brand with the same generic name. She’d misread it. With grounding techniques and a quick call to her GP, she got back on track.
These aren’t rare cases. They’re the norm.
The Bigger Picture
Drug safety alerts are increasing. In 2025, Australians received an average of 5.3 alerts per person annually-up from 1.9 in 2019. That’s not because drugs are less safe. It’s because monitoring is better. More data. Faster detection.
The goal isn’t to eliminate alerts. It’s to make sure you respond to them with your brain, not your fear.
By learning to pause, ground, assess, and consult-you’re not just avoiding panic. You’re becoming the kind of patient who gets better care. Who asks the right questions. Who stays in control.
This isn’t about being calm all the time. It’s about being capable when it matters most.
What should I do immediately after receiving a drug safety alert?
First, stop and breathe using the 4-7-8 technique: inhale for 4 seconds, hold for 7, exhale for 8. Do this three times. This calms your nervous system and restores rational thinking. Then, identify the source of the alert-was it from the TGA, FDA, or your pharmacist? Don’t stop your medication unless the alert explicitly says to. Contact your pharmacist next-they’re trained to interpret these alerts and can guide you safely.
Are drug safety alerts always urgent?
No. Most alerts are precautionary and affect only specific groups-like people with certain health conditions, older adults, or those taking other medications. A 2023 review found that 72% of alerts posed low or very low risk to the general population. Always check who the alert targets and whether it applies to you before taking action. Urgent alerts will use clear language like "immediate discontinuation" or "seek medical help now." If in doubt, call your pharmacist.
Can I rely on Google to understand a drug alert?
No. Google results often mix outdated information, anecdotal stories, and sensationalized headlines. An alert about a rare liver reaction might surface alongside someone’s personal fear story from 2018. Always go to official sources: the Therapeutic Goods Administration (TGA) website, your pharmacy’s alert notice, or your prescriber’s office. If you’re unsure, your pharmacist can help you find and interpret the real source.
Why is my pharmacist the best person to call first?
Pharmacists are trained to interpret drug safety alerts daily. They know which ones are critical, which are routine, and which are miscommunications. They can check your full medication history, spot potential interactions, and advise whether you need to switch, adjust, or continue. Calling your doctor might mean waiting days. Your pharmacist can often answer in minutes and may even have the updated prescribing guidelines on file.
How can I prepare for future drug safety alerts?
Create a simple alert response kit: keep a printed list of your current medications and doses, your pharmacist’s phone number, and a laminated card with the 4-7-8 breathing steps and 5-4-3-2-1 grounding technique. Practice the breathing and grounding exercises for 5 minutes a day for two weeks. This builds automaticity-so when an alert hits, your body knows what to do before your mind panics. Also, update your list every time your meds change.


Jason Jasper
25 12 25 / 14:07 PMBeen using the 4-7-8 trick since I read about it last year. Honestly, it’s the only thing that stops my hands from shaking when I get one of those emails from the pharmacy. Didn’t even know it had a name until now. Just breathed. Felt better. Didn’t panic. Didn’t stop my med. Just waited. Best 90 seconds of my day.
Still don’t know why I didn’t try this sooner.
Carlos Narvaez
26 12 25 / 18:29 PMMostly just people who don’t understand pharmacology trying to sound helpful. The 5-4-3-2-1 method? Cute. But if you’re on a drug with a narrow therapeutic index, breathing won’t fix a mislabeled batch. Real safety is in regulatory oversight, not mindfulness.
Harbans Singh
27 12 25 / 03:54 AMI live in India, and here, most people don’t even get alerts. We just get a new bottle with a different label and hope it’s the same thing. But I love how this post breaks it down. I printed the flowchart and stuck it on my fridge next to my insulin. My sister laughed-said I turned my medicine cabinet into a survival bunker. I told her, ‘Better safe than sorry.’
Also, the pharmacist thing? Huge. In Delhi, my local guy remembers my meds better than my doctor does. He’s my real health anchor.
Justin James
27 12 25 / 14:44 PMLet’s be real-these ‘safety alerts’ are just corporate cover-ups. Big Pharma knows their drugs are toxic but can’t admit it. The FDA? Controlled by lobbyists. The ‘low risk’ stats? Manufactured. That 72% number? Probably pulled from a study funded by the same company that made the drug.
And why do they push you to call your pharmacist? Because pharmacists are paid by the companies too. They’re the first line of damage control. They don’t want you to stop the drug-they want you to keep buying it.
I stopped all my meds after the last alert. Went organic. Started drinking colloidal silver. My blood pressure’s lower than ever. Coincidence? I think not.
They don’t want you to know this-but the real danger isn’t the drug. It’s the system that sells it to you while telling you to ‘breathe through it.’
Zabihullah Saleh
28 12 25 / 00:17 AMThis reminds me of something my grandfather used to say: ‘The body knows when it’s being lied to.’
He never took pills unless he understood why. Said if a doctor couldn’t explain it in plain terms, it wasn’t medicine-it was a gamble.
These steps? They’re not just about avoiding panic. They’re about reclaiming agency. In a world that treats us like data points, this is a quiet rebellion.
And honestly? The fact that you need a laminated card to not freak out when your body is being monitored… that’s the real tragedy here.
We’re not broken. The system is.
Winni Victor
28 12 25 / 09:25 AMUgh. So much virtue signaling wrapped in a bow. ‘Breathe and trust your pharmacist.’ Like that’s gonna fix the fact that half these drugs were approved because a lab rat died in week 3 and no one cared enough to follow up.
And don’t get me started on the ‘alert response kit.’ You’re turning your medicine cabinet into a Pinterest board. Next you’ll be buying scented candles for your statins.
Meanwhile, I’m just gonna Google it. At least I’m not paying for a therapist to teach me how to inhale.
Sophie Stallkind
30 12 25 / 08:25 AMWhile the emotional regulation techniques described are empirically supported and clinically validated, I must emphasize that their efficacy is contingent upon the patient’s baseline cognitive function and access to consistent healthcare infrastructure. Furthermore, the reliance on pharmacists as primary triage agents, while pragmatic in resource-constrained environments, may inadvertently undermine the physician-patient relationship, which remains the gold standard for individualized therapeutic decision-making.
That said, the 4-7-8 breathing protocol demonstrates measurable parasympathetic activation, as documented in the Journal of Clinical Psychology, 2021, and should be considered an adjunctive tool rather than a primary intervention.
sagar patel
31 12 25 / 08:57 AMI read this whole thing. You think breathing helps. It doesn't. I stopped my blood pressure med after an alert. Now I'm fine. No doctor. No pharmacist. Just me and my willpower.
Michael Dillon
1 01 26 / 22:57 PMOkay but have you ever tried this with a 3am alert when your kid’s sick and your pharmacy is closed and the website says ‘contact your prescriber’ but your doctor’s on vacation for two weeks?
I’ve been there. You don’t breathe. You don’t ground. You panic. You Google. You cry. You call your sister at 3am and she says ‘just keep taking it’ and you do.
This post is great. But it’s written for people who have time, access, and mental bandwidth. Most of us don’t.
So yeah-do the breathing. Do the checklist. But also-tell your reps to make the alerts actually useful. Not just scary headlines with a footnote that says ‘only applies to patients with renal impairment’ that’s buried in 12-point font.