This tool generates personalized monitoring schedules based on your condition status, reflecting current clinical guidelines for HSS and diabetes co-management.
Important: Always follow your healthcare provider's specific recommendations. This tool is for educational purposes only.
| Test | Frequency | Purpose |
|---|---|---|
| Echocardiogram | Every 6-12 months | Monitor septal thickness and LVOT gradient |
| HbA1c | Every 3 months | Track diabetes control and glucose management |
| Fasting Glucose | Every 3 months | Monitor daily glucose control |
| Blood Pressure | Every 1-3 months | Assess cardiovascular risk and medication effects |
| Lipid Panel | Every 3-6 months | Monitor cholesterol levels and cardiovascular risk |
| ECG | Every 6-12 months | Surveillance for arrhythmias |
Ever wondered why a heart condition and a blood‑sugar disorder sometimes show up together? It’s not a coincidence - hormones, genetics, and stress on the heart can link Hypertrophic Subaortic Stenosis (HSS) and diabetes in ways that matter for treatment and daily life.
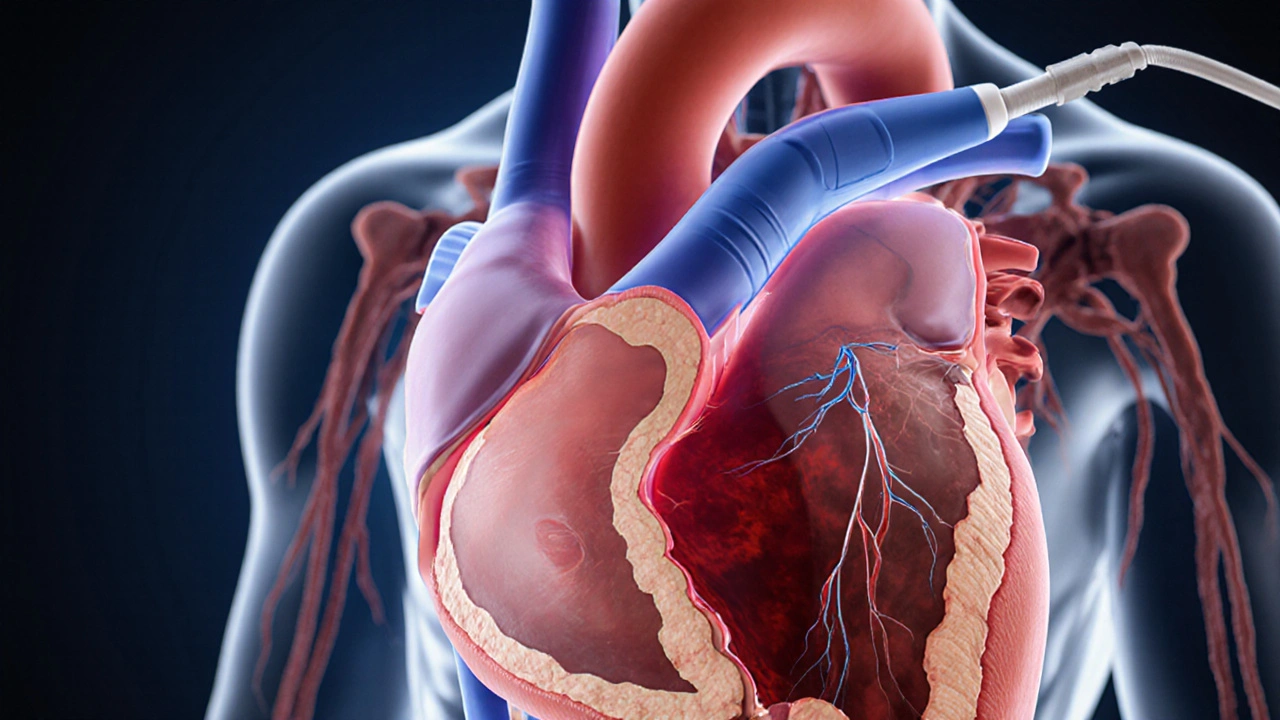
Hypertrophic Subaortic Stenosis is a form of hypertrophic cardiomyopathy where the heart’s septum thickens and blocks the outflow of blood from the left ventricle. The condition often appears in young adults and can cause chest pain, fainting, or sudden cardiac arrest. Diagnosis relies on echocardiography, which visualizes the thickened septum and measures the pressure gradient across the left ventricular outflow tract (LVOT). Treatment may involve beta‑blockers, calcium channel blockers, or procedural options like septal myectomy.
Diabetes-especially type2- is a chronic condition marked by elevated blood glucose due to insulin resistance or insufficient insulin production. Over time, high glucose damages blood vessels, nerves, and organs, raising the risk of heart disease, kidney failure, and vision loss. Key metrics include fasting plasma glucose, oral glucose tolerance test, and HbA1c. Management combines medication (metformin, SGLT2 inhibitors, insulin), diet, and exercise.
At first glance, a heart‑muscle disorder and a metabolic disease seem unrelated, but several mechanisms overlap:
These intersections mean that a patient with HSS who also develops diabetes faces a higher combined cardiovascular risk than either condition alone.
Because the overlap amplifies danger, clinicians follow a tighter monitoring schedule:
When both conditions coexist, treatment goals tighten: aim for an HbA1c <7% (or individualized target) while keeping the LVOT gradient below 30mmHg to avoid symptoms.
Several strategies hit both the heart and sugar levels:
| Therapy | Effect on HSS | Effect on Diabetes |
|---|---|---|
| Beta‑blockers | Reduce heart rate, lower LVOT gradient | May blunt hypoglycemia awareness, require dose adjustment |
| ACE inhibitors/ARBs | Improve ventricular remodeling | Protect kidneys, improve insulin sensitivity |
| Regular aerobic exercise | Enhances myocardial oxygen demand balance | Improves glucose uptake and insulin sensitivity |
| SGLT2 inhibitors | Reduce cardiac preload, modest reduction in LV mass | Lower blood glucose and promote weight loss |
| Dietary sodium restriction | Decreases afterload, lessening obstruction | Supports blood‑pressure control, aids glycemic stability |
Note: Not every drug works for everyone. For example, beta‑blockers can mask signs of low blood sugar, so patients need careful education.
If you experience any of the following, treat it as an emergency:
Call emergency services right away; early intervention can save both heart muscle and life.
Diabetes doesn’t directly cause the septal thickening seen in HSS, but chronic high blood sugar accelerates fibrosis and myocardial stiffness, which can worsen an existing obstruction.
Yes. Studies from 2023-2024 show a 1.8‑fold increase in sudden cardiac death among patients with both HSS and poorly controlled diabetes compared to HSS alone.
Beta‑blockers can mask early warning signs of hypoglycemia, making it harder to detect low glucose. They may also slightly raise HbA1c, so doctors often adjust diabetes meds when prescribing them.
If you have a family history of HSS, unexplained chest pain, or abnormal ECG findings, an echocardiogram is advisable-even if you only have diabetes.
SGLT2 inhibitors (e.g., empagliflozin) have shown modest reductions in left‑ventricular mass and improve glycemic control, making them a promising option for patients with both HSS and type2 diabetes.
Understanding the link between Hypertrophic Subaortic Stenosis and diabetes helps you stay ahead of complications. By keeping an eye on heart imaging, blood‑sugar numbers, and lifestyle habits, you can reduce risk and enjoy a fuller life.
michael klinger
12 10 25 / 06:06 AMThe whole HSS‑diabetes link is just another hidden agenda cooked up by Big Pharma to sell more meds.
Matt Laferty
15 10 25 / 08:46 AMWhen you look at the data, the overlap between hypertrophic subaortic stenosis and type‑2 diabetes is striking.
Both conditions share a common thread of insulin resistance that seems to accelerate myocardial remodeling.
Chronic hyperglycemia fuels the formation of advanced glycation end‑products, which in turn stiffen the ventricular septum.
This mechanical stiffening magnifies the LVOT gradient, pushing patients closer to symptomatic obstruction.
On the flip side, the hypertrophic myocardium itself can impair peripheral glucose uptake, creating a vicious feedback loop.
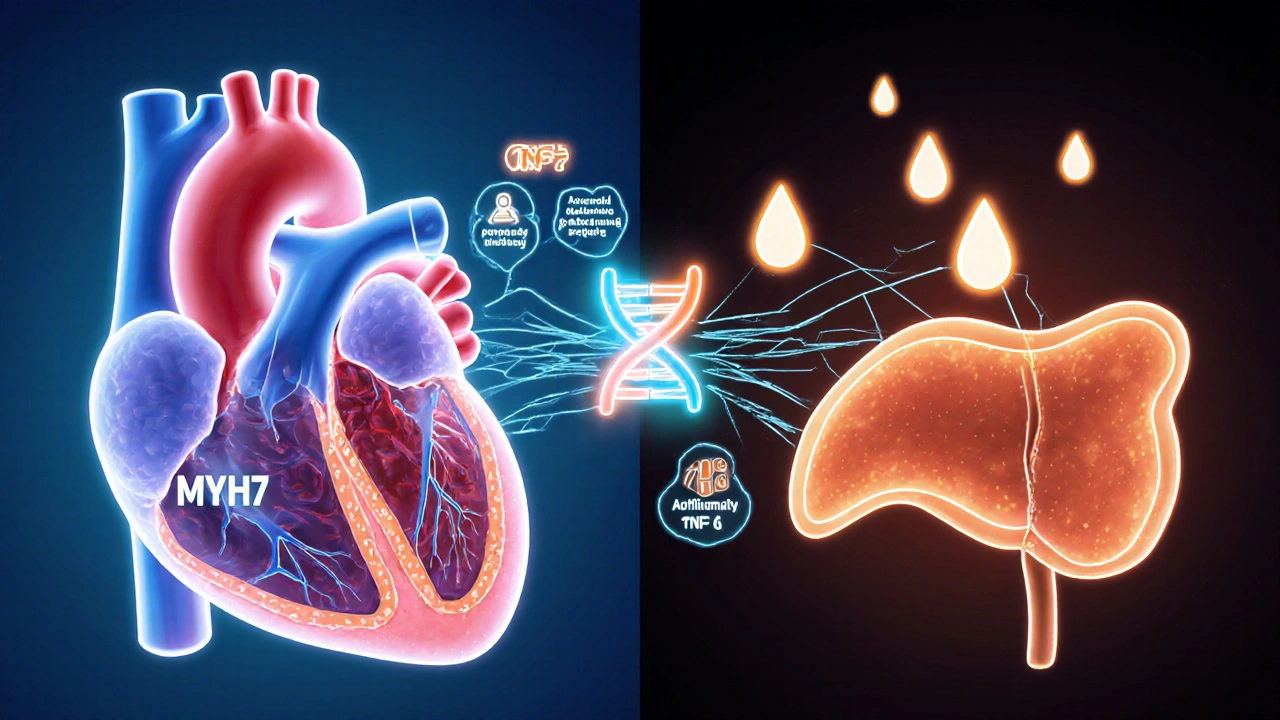
Genetic studies have identified MYH7 mutations that not only thicken the heart muscle but also disrupt normal insulin signaling pathways.
Inflammatory cytokines such as TNF‑α and IL‑6 are elevated in both diseases, promoting fibrosis and worsening cardiac output.
From a clinical perspective, this means that a patient who suddenly develops worsening dyspnea should also be screened for glucose intolerance.
Conversely, a diabetic whose HbA1c jumps above 8 % should get an echocardiogram even if they have no chest pain.
Standard monitoring schedules recommend an echocardiogram every six to twelve months for high‑risk HSS patients.
Adding quarterly HbA1c and fasting glucose tests allows early detection of metabolic decompensation.
Blood pressure and lipid panels every three to six months keep the vascular load in check.
Electrocardiograms every six to twelve months catch arrhythmias that beta‑blockers might mask.
Therapeutically, tight glycemic control with SGLT2 inhibitors has been shown to reduce left‑ventricular hypertrophy in some studies.
Beta‑blockers and calcium‑channel blockers remain first‑line for gradient reduction, but they must be dosed carefully in diabetics to avoid hypoglycemia.
In short, treating HSS and diabetes as separate entities is a missed opportunity; an integrated care plan saves lives and improves quality of life.
Genie Herron
18 10 25 / 11:26 AMWow this whole thing just feels like a punch to the gut it’s scary how the heart and sugar levels can mess with each other and I keep thinking about how many people suffer silently without even knowing it I wish there was a simple fix but the reality is harsh and confusing
Danielle Spence
21 10 25 / 14:06 PMThe way we ignore lifestyle choices when faced with HSS and diabetes is downright irresponsible. People need to own up to their diet and activity levels before blaming genetics alone. It's a matter of personal accountability and public health.
Taryn Thompson
24 10 25 / 16:46 PMThe recommended monitoring schedule you see in the article reflects current consensus guidelines. An echocardiogram every six to twelve months allows clinicians to track septal thickness and LVOT gradients objectively. Quarterly HbA1c measurements are essential to assess glucose control, especially because fluctuations can directly affect myocardial compliance. Blood pressure checks every one to three months help titrate antihypertensive therapy without precipitating orthostatic episodes. Lipid panels at three‑ to six‑month intervals keep a watch on atherogenic risk, which is amplified when HSS and diabetes coexist. Finally, an annual ECG serves as a safety net for detecting arrhythmias that may be silent until they become life‑threatening.
Lisa Lower
27 10 25 / 18:26 PMListen up you can take charge of this combo condition by staying on top of your checks. Schedule that echo and never skip the HbA1c test because consistency wins. Keep your blood pressure in the green zone and watch your cholesterol like a hawk. Exercise daily even if it’s just a brisk walk and track your carbs meticulously. Remember each small win adds up to big health gains.
Dana Sellers
30 10 25 / 21:06 PMIt’s pretty obvious that folks who binge on junk food are asking for trouble with both heart and sugar problems. Stop making excuses and start eating real food.
Damon Farnham
2 11 25 / 23:46 PMPatriots of true health must reject the globalist agenda that pushes sugary processed foods onto our plates, for it is a calculated assault on our cardiovascular sovereignty; the very same entities that profit from pharmaceutical interventions also thrive on our neglect, and they will stop at nothing to keep us dependent on their insidious drugs; therefore, we must champion home‑grown, nutrient‑dense meals and demand rigorous screening for conditions like HSS and diabetes, lest we fall prey to their nefarious schemes.
Gary Tynes
6 11 25 / 02:26 AMHey buddy i get that juggling heart checks and sugar numbers can feel overwhelming but you got this keep that schedule handy and set reminders on your phone it’ll make things way easier dont forget to reward yourself when you hit those goals keep pushing forward
Marsha Saminathan
9 11 25 / 05:06 AMAlright team imagine your body as a high‑performance race car and the heart is the engine that needs premium fuel and regular tune‑ups you don’t want cheap gasoline messing with the pistons so keep that blood sugar in check with smart meals and steady exercise plus the echo appointments are like pit stops that ensure the engine’s valves aren’t wearing out and the lipid panels are the oil checks that keep everything running smooth keep your schedule tight stay disciplined and watch how your performance skyrockets
Justin Park
12 11 25 / 07:46 AM🤔 The intertwining of HSS and diabetes invites us to ponder the delicate balance between mechanical function and metabolic harmony. When one system falters, the other feels the ripple, reminding us that health is a holistic tapestry.
Herman Rochelle
15 11 25 / 10:26 AMI’m proud of anyone who sticks to the monitoring plan – each appointment is a step toward stability and peace of mind.
Stanley Platt
18 11 25 / 13:06 PMIt is incumbent upon healthcare professionals to adopt an interdisciplinary approach, whereby cardiologists and endocrinologists collaboratively devise individualized surveillance protocols; such synergy not only optimizes clinical outcomes but also fosters patient empowerment through education and shared decision‑making.
Alice Settineri
21 11 25 / 15:46 PMWow, you’re really missing the point here – it’s not just about numbers, it’s about living your best freaking life, so ditch the boring charts and actually enjoy the freedom a well‑managed regimen gives you!
nathaniel stewart
24 11 25 / 18:26 PMCongratulations on taking the first step toward mastering your health; with perseverance and a dash of optimism, you will navigate the complexities of HSS and diabetes with grace and success.
Pathan Jahidkhan
27 11 25 / 21:06 PMOne could argue that the whole monitoring regime is just a bureaucratic circus designed to keep patients in perpetual anxiety but maybe there’s a grain of truth hidden under the paperwork
Dustin Hardage
30 11 25 / 23:46 PMFrom a pathophysiological standpoint, the convergence of left ventricular outflow tract obstruction and insulin resistance warrants a synchronized therapeutic strategy; integrating beta‑blockade with agents that improve glycemic control addresses both hemodynamic load and metabolic stress, thereby mitigating progressive myocardial fibrosis.
Dawson Turcott
4 12 25 / 02:26 AMSure, because adding another lab test is exactly what my weekend needed 😂 but hey if it keeps the heart from throwing a fit, I’ll sign up for the parade.
Alex Jhonson
7 12 25 / 05:06 AMLet’s remember that every data point, from echo to HbA1c, is a brushstroke in the larger portrait of patient wellness; respecting each measurement helps us paint a clearer picture together.