Medication Risk Checker
Check Your Medication Safety
This tool checks if your medications are high-risk for older adults according to the Beers Criteria, the gold standard for safe prescribing in seniors. Enter your medications below to see if any require review with your doctor.
Important: This tool is for informational purposes only. Always consult your healthcare provider before making any changes to your medications.
What This Means
Medications are categorized based on Beers Criteria:
High Risk - Should be avoided or used with extreme caution
(e.g., long-term benzodiazepines, anticholinergics, certain NSAIDs)
Medium Risk - Should be used with dose adjustments or monitoring
(e.g., some antihypertensives, certain antidepressants)
Low Risk - Generally safe for older adults with standard dosing
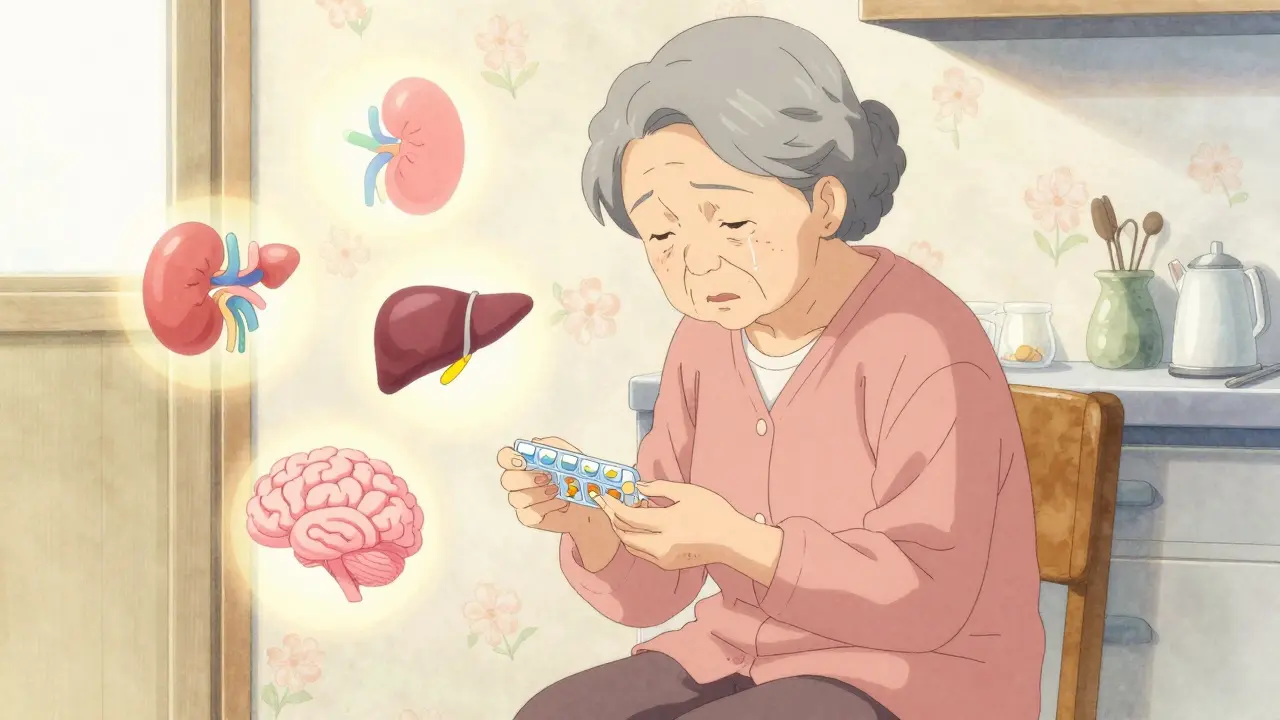
When you’re 80, a pill that worked fine at 50 can leave you dizzy, confused, or even hospitalized. It’s not that the medicine changed. It’s that your body did.
Why Older Bodies Handle Drugs Differently
As you age, your body changes in ways that directly affect how medications work. These aren’t minor tweaks-they’re major shifts in how drugs are absorbed, moved around, broken down, and cleared from your system. By age 65, your kidneys are already filtering blood 30-50% slower than they did in your 30s. That means drugs like digoxin, lithium, or certain antibiotics stick around longer, building up to dangerous levels even if you take the same dose you always have.
Your liver isn’t working as hard either. Blood flow to the liver drops by 20-40% between ages 25 and 65. That slows down the breakdown of drugs like propranolol and verapamil, making them stronger and longer-lasting than expected. At the same time, your body composition changes. You lose about 15% of your total water and gain up to 13% more body fat. That means water-soluble drugs (like some diuretics) become more concentrated in your bloodstream, while fat-soluble drugs (like diazepam) get stored in fat tissue and released slowly, causing prolonged effects.
Then there’s protein binding. Older adults often have lower levels of albumin, the main protein that carries drugs like warfarin through the blood. With less albumin, more of the drug floats around freely-unbound-and that’s the active, dangerous part. A normal dose of warfarin can suddenly become a bleeding risk because your body can’t hold it in check like it used to.
Brain and Heart Become More Sensitive
It’s not just about how your body processes drugs-it’s about how your organs respond to them. Your brain becomes far more sensitive to sedatives. A dose of diazepam that barely makes a 30-year-old sleepy can cause serious confusion, memory loss, or even delirium in someone over 75. Studies show older adults experience 50% more sedation and cognitive impairment at the same blood levels as younger people.
Your heart reacts differently too. Beta-blockers like propranolol need 50% higher doses in younger adults to slow the heart rate. But in older adults, even low doses can cause dangerously low blood pressure or a slow pulse. That’s why a medication prescribed for heart rhythm or high blood pressure can accidentally make you feel weak, faint, or fall.
Anticholinergic drugs-commonly found in allergy meds, sleep aids, and some antidepressants-are especially risky. These block a brain chemical called acetylcholine, which helps with memory and focus. In older adults, even small amounts can trigger confusion, hallucinations, or urinary retention. One 2023 study found people over 75 were 4.2 times more likely to develop delirium from these drugs than those under 65.
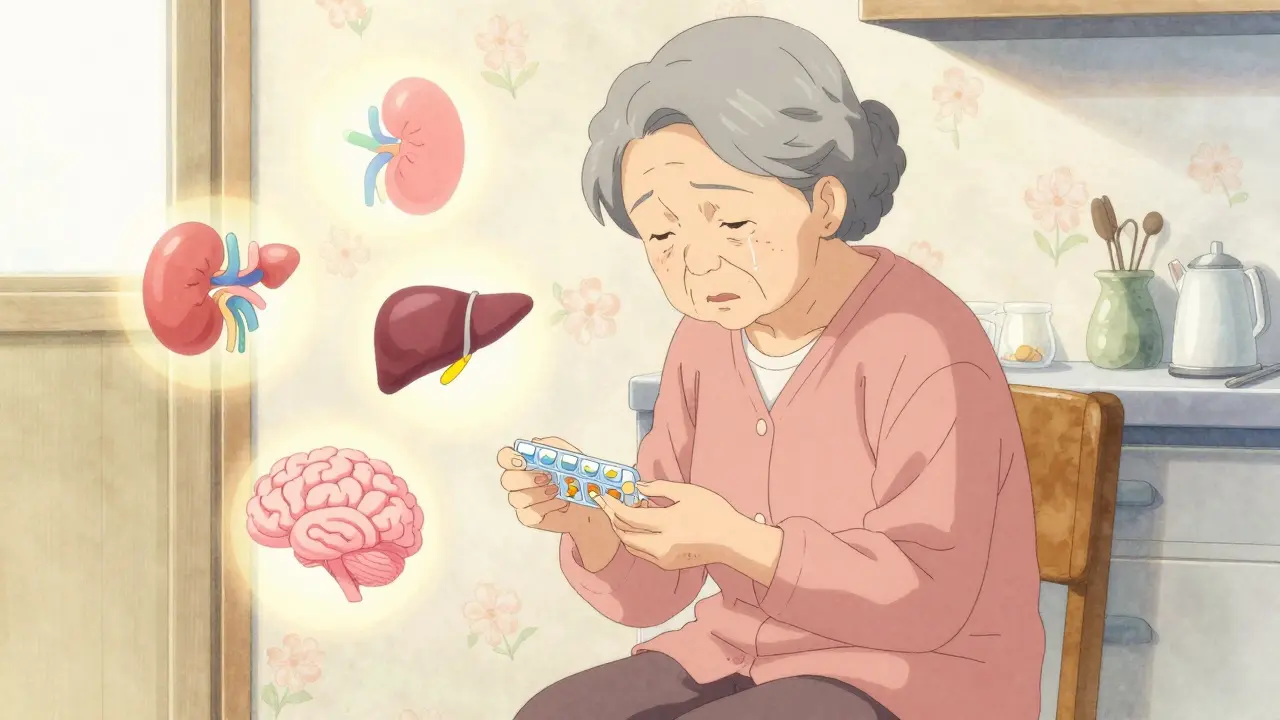
The Polypharmacy Trap
Nearly half of adults over 65 take five or more prescription drugs every month. That’s called polypharmacy-and it’s a minefield. Each new medication adds another layer of risk. One drug might slow kidney function, making another drug build up. A third might increase drowsiness, making falls more likely. And many of these prescriptions come from different doctors, with no one looking at the whole picture.
The result? A 2022 survey of older adults found that 68% had experienced dizziness or falls linked to their meds. More than half reported memory problems or confusion. And 45% admitted they’d stopped taking a drug because the side effects were worse than the condition it was meant to treat.
The Beers Criteria, updated every two years by the American Geriatrics Society, lists 56 medications that are too risky for older adults. These include common drugs like diphenhydramine (Benadryl), benzodiazepines (Valium, Xanax), and certain NSAIDs. Even if your doctor didn’t know about the list, the risks are real. One study showed that 42% of older adults were taking at least one of these dangerous drugs-and 15% had suffered a related adverse event.
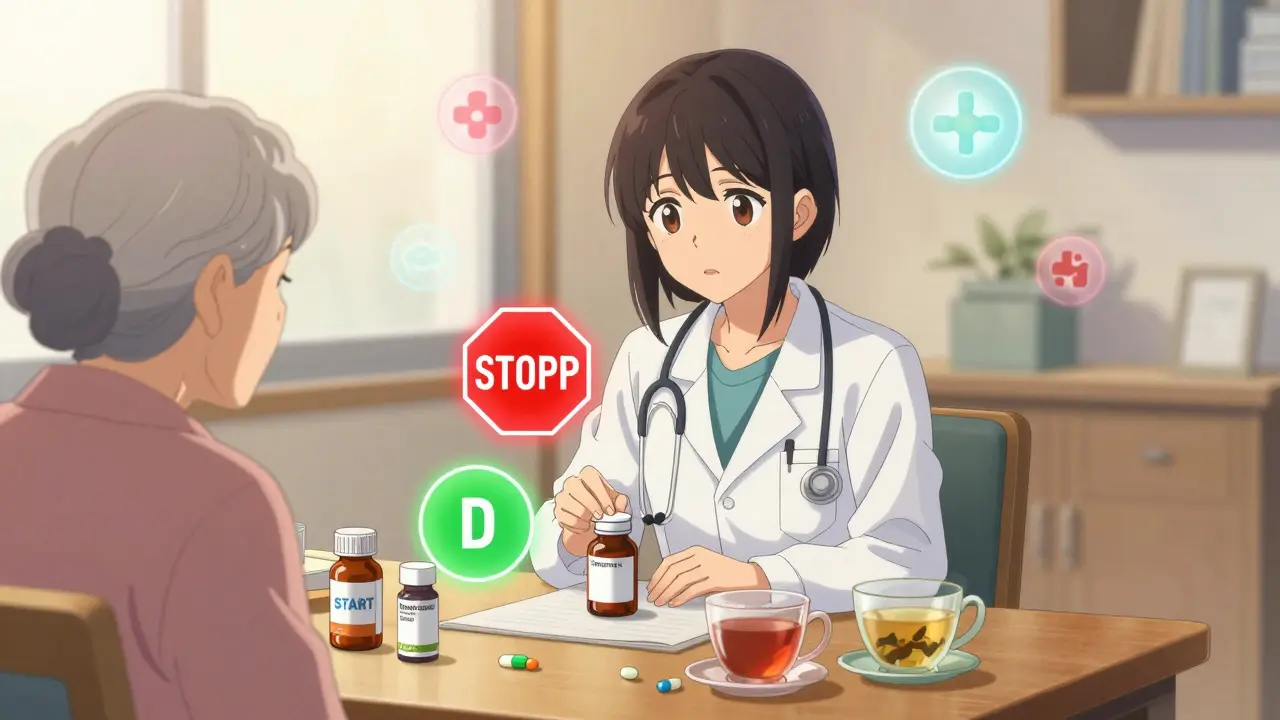
What Doctors Should Be Doing
The solution isn’t to stop all meds. It’s to use them smarter. The standard advice is simple:
start low, go slow. That means beginning with 25-50% of the usual adult dose, especially for drugs cleared by the kidneys. A 70-year-old on a blood thinner might need half the dose of a 45-year-old. A sleep aid might be cut to a quarter of the standard tablet.
Regular medication reviews are critical. Every 3-6 months, your doctor should go through every pill, patch, and supplement you’re taking. This is called a Brown Bag Review-bring everything you use, including over-the-counter drugs and herbal products. Studies show this uncovers an average of 3.2 medication errors per person.
The STOPP/START criteria, developed by geriatric experts, help doctors decide what to stop and what to start. STOPP flags inappropriate drugs (like long-term benzodiazepines). START reminds them to prescribe things older adults often miss-like vitamin D, flu shots, or bone-strengthening meds. Hospitals that use these tools see a 22% drop in adverse drug events.
Real Stories, Real Consequences
One 82-year-old woman was prescribed a standard dose of a blood pressure medication that worked fine for her 50-year-old neighbor. Within weeks, she fell and broke her hip. Her doctor hadn’t adjusted the dose for her age, kidney function, or weight. Her story isn’t rare. In fact, a 2023 study found that 37% of adults over 80 had been hospitalized due to medication side effects-and 62% of those cases were preventable.
Another man, 78, started amitriptyline for nerve pain. Within three days, he couldn’t urinate. He needed a catheter. His doctor didn’t realize that amitriptyline is a strong anticholinergic-and that men his age with enlarged prostates are at high risk for this exact side effect.
These aren’t mistakes. They’re systemic failures. Clinical trials rarely include people over 75. So most drug dosing guidelines are based on data from people decades younger. That’s like prescribing a child’s car seat to a 6-foot-4 adult. It doesn’t fit. It doesn’t protect. And it can hurt.
What You Can Do
You don’t have to wait for your doctor to bring it up. Ask these questions at every appointment:
- Is this medication still necessary? (Many are prescribed years ago and never reviewed.)
- Could this be causing my dizziness, confusion, or constipation?
- Can we try a lower dose?
- Is there a safer alternative on the Beers Criteria list?
- Can we stop one of my other meds to make room for this one?
Bring a list of every medication-including vitamins, supplements, and herbal teas. Many older adults take melatonin, St. John’s wort, or ginkgo biloba, which can interact badly with prescription drugs.
Ask for a kidney function test (eGFR). If your eGFR is below 60, your doses likely need adjustment. Don’t assume your doctor knows your numbers-ask for them.
And if you’re feeling worse after starting a new drug, don’t just tough it out. Call your doctor. That dizziness? That foggy brain? That constipation? Those aren’t normal signs of aging. They’re warning signs.
The Future Is Personalized
New tools are emerging to make geriatric prescribing smarter. Pharmacogenomic testing can now tell you how your genes break down certain drugs-like antidepressants or blood thinners. One 2023 study found this testing cut adverse reactions by 35% in older adults.
Artificial intelligence tools like MedAware are being used in hospitals to flag dangerous drug combinations before they’re prescribed. The FDA now encourages including more older adults in clinical trials. And by 2026, Medicare may require a full medication review for every beneficiary.
The goal isn’t to eliminate meds. It’s to match them to the person. Your body isn’t a 30-year-old’s body. Your meds shouldn’t be either.
Why do older adults have more side effects from the same dose of medication?
Older adults have slower kidney and liver function, less body water, more body fat, and lower protein levels-all of which change how drugs are absorbed, distributed, and cleared. Their brains and hearts also become more sensitive to medications. A dose that’s safe for a 40-year-old can be toxic for an 80-year-old because their body doesn’t handle it the same way.
What are the most dangerous medications for older adults?
According to the 2023 Beers Criteria, the most dangerous include benzodiazepines (like diazepam), anticholinergics (like diphenhydramine), non-steroidal anti-inflammatory drugs (NSAIDs), and certain sleep aids like zolpidem. These drugs increase risks of falls, confusion, kidney damage, and bleeding. Some, like meperidine and long-term benzodiazepines, should be avoided entirely in older adults.
How many medications are too many for someone over 65?
There’s no magic number, but taking five or more medications (polypharmacy) significantly raises the risk of side effects and interactions. Studies show 48% of adults over 65 take five or more prescriptions. The key isn’t just the count-it’s whether each drug is still needed, at the right dose, and not causing harm. Regular reviews can cut unnecessary meds by 20-30%.
Can you stop taking medications safely as you get older?
Yes-and it’s often safer than continuing. This is called deprescribing. Many drugs prescribed years ago for conditions like high cholesterol or mild hypertension may no longer be needed, especially if goals of care have shifted toward comfort and quality of life. Stopping one drug can reduce side effects, improve cognition, and lower fall risk. Always do this under medical supervision, never on your own.
What should I bring to my medication review appointment?
Bring everything you take: prescription pills, over-the-counter meds (like pain relievers or sleep aids), vitamins, herbal supplements, and even topical creams or patches. Many interactions happen with things you think are harmless. A Brown Bag Review-where you bring all your meds in a bag to your appointment-helps your doctor see the full picture and spot duplicates, outdated prescriptions, or dangerous combinations.
Are there tests to help determine the right medication dose for older adults?
Yes. A simple blood test called eGFR (estimated glomerular filtration rate) shows how well your kidneys are working-and that’s critical for dosing many drugs. Pharmacogenomic tests can also reveal how your body metabolizes certain medications, especially antidepressants and blood thinners. These tests aren’t routine yet, but they’re becoming more common and can prevent dangerous side effects.
If you’re caring for an older adult, pay attention to changes in behavior, balance, or appetite after a new medication starts. A fall, confusion, or sudden weight loss could be a drug reaction-not just aging. Ask questions. Push for reviews. And remember: just because a pill has been prescribed doesn’t mean it still belongs in the medicine cabinet.
Erwin Kodiat
19 01 26 / 13:17 PMBeen watching my dad go through this for years. He was on six meds at 78, then we did a brown bag review and cut three. Suddenly he was walking without a cane, remembering birthdays, and even started gardening again. It’s not magic-it’s just paying attention. Doctors don’t always see the whole picture, but family can. Don’t assume side effects are just ‘getting older.’
Malikah Rajap
19 01 26 / 17:30 PMSo... let me get this straight-your body’s like a rusty old car, and the meds are gasoline? And if you don’t adjust the fuel line, you’re gonna blow the engine? I mean... wow. I never thought of it that way. I just thought Grandma was being dramatic when she said the pills made her feel like she was floating through a fog. Turns out, she was just chemically overdosed by a system designed for 30-year-olds. Sad. And terrifying.
Aman Kumar
20 01 26 / 05:14 AMLet’s be brutally honest: the pharmaceutical-industrial complex has weaponized geriatric neglect. Clinical trials exclude the elderly because they’re ‘complicated’-which is code for ‘not profitable.’ The FDA’s guidelines are written by men who’ve never held an 82-year-old’s hand while they try to swallow a pill that makes them vomit. The Beers Criteria? A band-aid on a hemorrhage. We need systemic overhaul-not ‘start low, go slow.’ We need liability reform, mandatory geriatric pharmacology training for every prescriber, and zero tolerance for off-label polypharmacy. This isn’t medicine. It’s elder exploitation dressed in white coats.
Phil Hillson
20 01 26 / 08:48 AMBro just stopped all his meds and now he's fine
Tracy Howard
20 01 26 / 21:59 PMCan we just acknowledge that American healthcare is a carnival ride where the elderly are the clowns? We pump them full of drugs designed for people half their age, then act shocked when they collapse. Meanwhile, Canada and the UK have national geriatric prescribing protocols. We don’t. We have Dr. Google and a 7-minute visit. It’s not negligence-it’s cultural contempt wrapped in insurance forms. And don’t get me started on how Medicare reimburses for prescribing, not for reviewing. This isn’t a medical crisis. It’s a moral one.
sujit paul
22 01 26 / 13:39 PMThere is a deeper metaphysical truth here: the body is not a machine to be calibrated, but a temple in decay. Modern medicine treats aging as a bug to be patched, when in fact it is the natural rhythm of dissolution. The pills are not the problem-they are the symptom of our denial. We refuse to accept mortality, so we drown ourselves in chemistry. The real cure is not lower doses-it is surrender. To time. To silence. To the quiet letting go. The elderly do not need more science. They need more reverence.
Lewis Yeaple
22 01 26 / 16:05 PMIt’s worth noting that the pharmacokinetic changes referenced in the post-reduced renal clearance, decreased hepatic metabolism, altered body composition-are well-documented in peer-reviewed literature since the 1980s. The fact that these principles are still not universally applied reflects a systemic failure in medical education and clinical workflow, not a lack of evidence. The Beers Criteria are evidence-based, yet compliance rates among primary care providers remain below 30%. This is not ignorance-it’s institutional inertia.
Jackson Doughart
23 01 26 / 04:45 AMI’ve been a geriatric nurse for 24 years. I’ve seen the same mistakes over and over. A man on warfarin, no INR checks for six months. A woman on Benadryl for insomnia since 1998. A husband who didn’t tell his cardiologist about the OTC sleep aid because he thought it was ‘just herbal.’ These aren’t edge cases. They’re the norm. The solution isn’t complicated: listen. Ask. Review. Repeat. It takes five minutes. But in our rushed system, five minutes is a luxury. I wish more people knew: sometimes, the most powerful medicine is silence-and the courage to say, ‘Let’s stop this.’