
Most people assume the United States pays the most for everything medical - and they’re right about brand-name drugs. But here’s the twist: when it comes to generic drug prices, Americans often pay less than people in Europe. It sounds backwards, but it’s true. A 2022 analysis from the U.S. Department of Health and Human Services found that generic drugs in the U.S. cost, on average, 33% less than in 33 other wealthy nations. Meanwhile, the same report showed Americans pay more than three times the price for brand-name drugs compared to Europeans. So why does this happen? And how can the same country have both the cheapest generics and the most expensive brand-name medicines in the world?
How the U.S. Generic Market Works
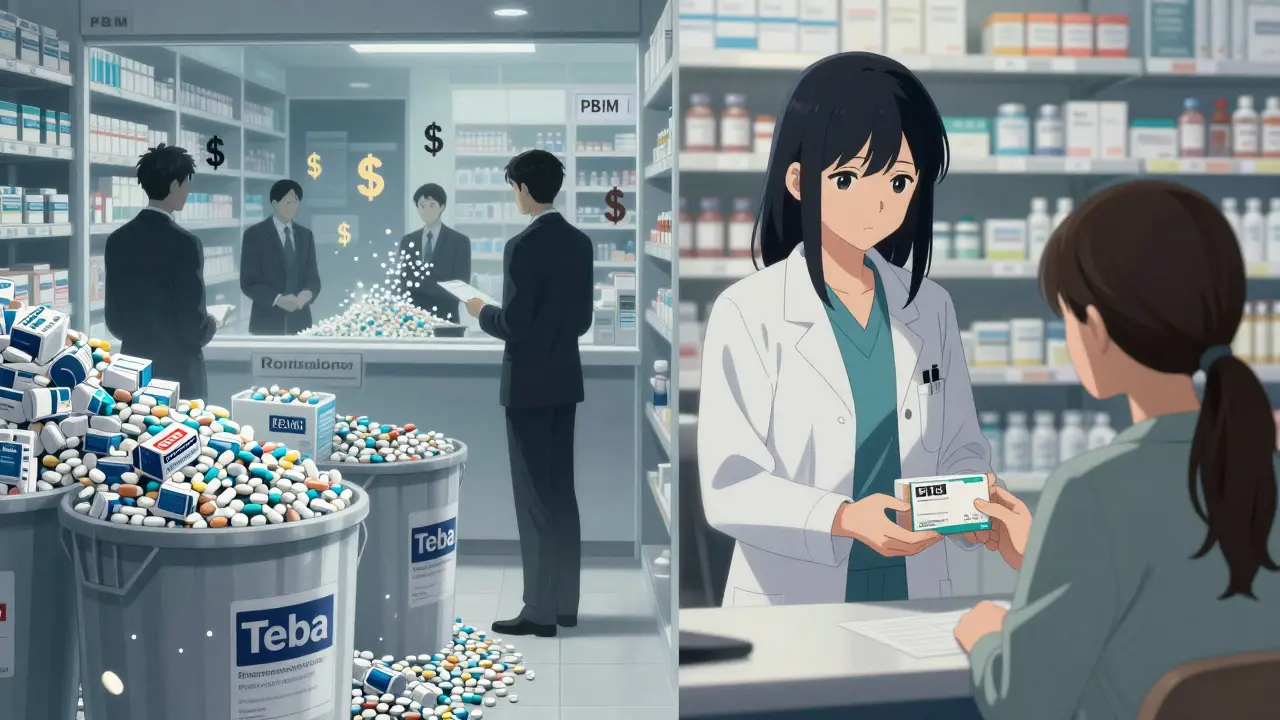
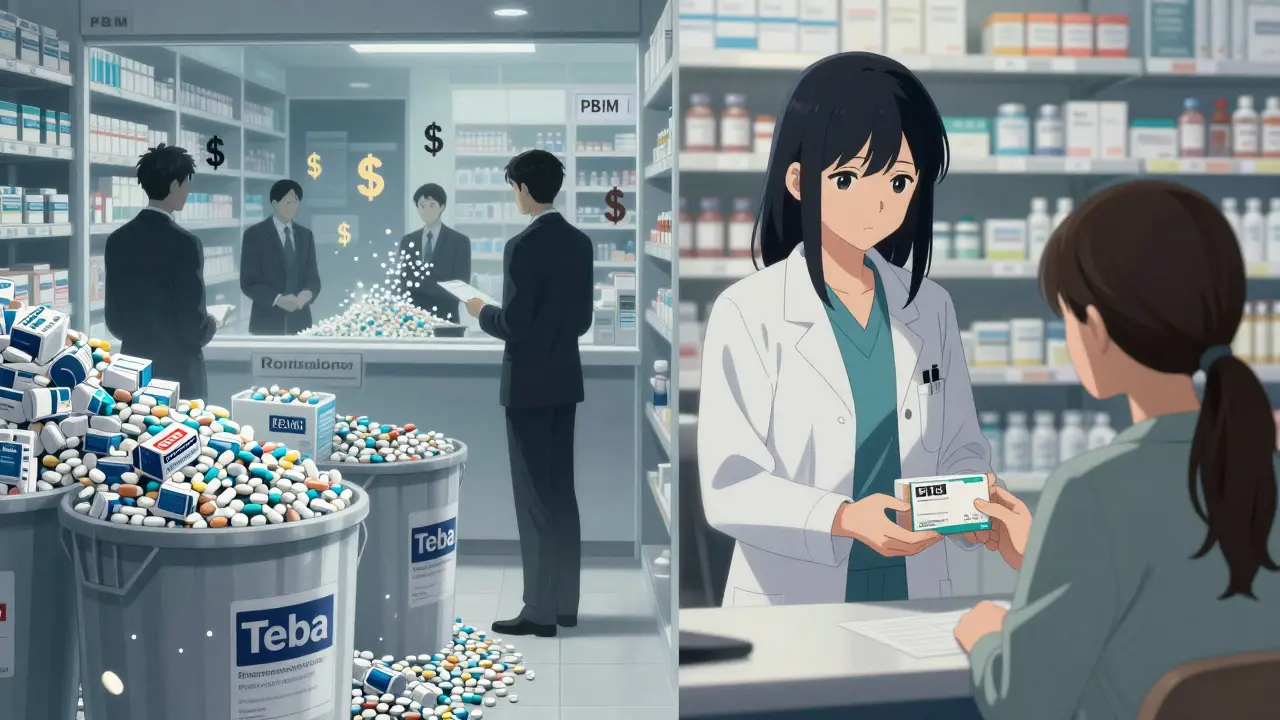
The U.S. generic drug market isn’t just competitive - it’s brutal. Once a brand-name drug loses its patent, dozens of companies jump in to make copies. Companies like Teva, Mylan, and Sandoz produce pills by the billions. With so many suppliers, prices drop fast. In some cases, the cost of making a generic pill is less than a penny. But because pharmacies and Pharmacy Benefit Managers (PBMs) buy in massive volumes, they squeeze suppliers even harder. The result? A 30-day supply of generic lisinopril, used for high blood pressure, can cost as little as $4 at Walmart - sometimes even $0 with insurance.
This isn’t luck. It’s structure. The U.S. has no central price setter. Instead, PBMs - middlemen who manage drug benefits for insurers - negotiate discounts behind the scenes. They don’t always pass those savings to patients, but they do force manufacturers to slash prices just to stay in the game. If a company doesn’t offer the lowest bid, it gets kicked off formularies. That’s why some generic drugs sell below cost. Producers stay in the game hoping to make up losses on other products. But when too many companies exit because profits vanish, shortages happen. That’s when one supplier can raise prices - and they do. It’s a cycle: too low, then too high.
How Europe Handles Generic Drugs
In Europe, the system is the opposite. Governments set prices. In Germany, France, and the UK, health agencies decide how much a drug should cost based on what it’s worth medically - not how much companies want to charge. This sounds fair, but it creates a different problem: less competition. Only about 41% of prescriptions in Europe are for generic drugs, compared to 90% in the U.S. Why? Because European regulators don’t push pharmacists to substitute generics automatically. In France, a doctor has to approve every switch from brand to generic. In Germany, pharmacists can swap, but many patients stick with what’s prescribed.
Also, European manufacturers don’t face the same pressure to undercut each other. There’s no giant PBM system forcing volume-based discounts. Instead, governments use “reference pricing” - they look at what other countries pay and set their own price accordingly. If the UK pays $10 for a generic, Germany won’t pay more than $12. That keeps prices stable, but it also keeps them higher. A 2025 study in the
JAMA Health Forum showed that the average price index for generics in the U.S. was 298.2, while Germany’s was 98.7 - meaning U.S. list prices looked higher. But that number doesn’t include the rebates and discounts hidden in the U.S. system. Once you factor those in, net U.S. prices drop below Europe’s.
Why Brand-Name Drugs Cost So Much More in the U.S.
The real imbalance isn’t in generics - it’s in brand-name drugs. The U.S. pays 422% more for new medicines than other OECD countries. That’s not because Americans are greedy. It’s because the system is built to pay more. Pharmaceutical companies charge high prices in the U.S. to fund research. About two-thirds of all global drug development is paid for by American consumers. The rest of the world benefits from lower prices, but they don’t pay the upfront cost of discovery.
Take Jardiance, a diabetes drug. In the U.S., Medicare negotiated a price of $204 per month. In other countries, the average was $52. That’s almost four times more. But that’s still less than the original list price - which was over $500. The difference? Rebates. PBMs get 35-40% off list prices, but patients don’t see that. They pay whatever their insurance co-pay says - which is often still hundreds of dollars. Meanwhile, in Germany, the government negotiates a single price for the whole country. No rebates. No hidden discounts. Just one price everyone pays. That’s why Europeans are shocked when they visit the U.S. and see $4 generic pills - but also why Americans are stunned when they travel to Europe and pay €15 for the same pill.
Who Pays the Real Price?
It’s easy to say Americans are getting a deal on generics. But the full picture is more complicated. The U.S. spends $1,443 per person on pharmaceuticals each year. Germany spends $749. The UK spends $512. That’s not because Americans take more medicine - they take about the same amount. It’s because they pay more for the new stuff. The trade-off is this: the U.S. funds the future. Most new drugs - cancer treatments, rare disease therapies, weight-loss drugs like Wegovy - are first developed and tested in the U.S. because companies know they can recover their costs here.
European countries, with their strict price controls, often delay access to new drugs. NICE in the UK may reject a drug if it’s too expensive relative to its benefit. That saves money, but it also means patients wait longer - or don’t get the drug at all. Meanwhile, Americans get access faster, but pay more out of pocket. A 2024 survey by the European Patients’ Forum found 78% of Europeans thought U.S. brand-name prices were “unjustifiably high.” But they also benefit from the innovation that comes from those high prices.
What’s Changing?
The U.S. is starting to change. The Inflation Reduction Act lets Medicare negotiate prices for 10 high-cost brand-name drugs. For the first time, the government is stepping in to cap prices. In 2024, Medicare’s negotiated price for Stelara was $4,490 - still higher than the $2,822 average elsewhere, but down from over $7,000. That’s a start. But experts warn this could backfire. If the U.S. cuts prices too much, drug companies might raise prices elsewhere to make up the difference. Alexander Natz of the European Confederation of Pharmaceutical Entrepreneurs warned in late 2025 that a “most favored nation” pricing policy - where the U.S. matches the lowest global price - could force manufacturers to hike prices in Europe by up to 20% to protect profits.
At the same time, the U.S. generic market is under pressure. With profit margins so thin, some manufacturers are leaving. In 2024, shortages hit 140 generic drugs - from antibiotics to heart medications. The FDA says it’s partly because the system rewards low prices over reliability. Companies don’t invest in quality or backup supply chains if they’re barely breaking even.

What This Means for You
If you’re in the U.S. and take generics, you’re getting one of the best deals in global health care. A month’s supply of metformin? $4. Generic ibuprofen? $2. That’s not a fluke. It’s the result of a hyper-competitive, volume-driven market. But if you need a new, patented drug, you’re in a different world. You’re paying for the research that makes those generics possible - and you’re paying more than anyone else.
If you’re in Europe, you pay less for brand-name drugs, but more for generics. You get access to medicines, but sometimes slower. And you’re not paying for the innovation that happens in the U.S. - someone else is.
The truth? Neither system is perfect. The U.S. has efficiency but instability. Europe has fairness but slower access. And the global pharmaceutical system is built on a quiet bargain: Americans pay high prices for new drugs so the rest of the world can afford older ones. That bargain is now under strain. As Medicare negotiates prices and other countries push back, that balance could shift - and no one knows exactly how it will end.
What You Can Do
If you’re in the U.S. and take generics:
- Always ask if a generic is available - even if your doctor didn’t prescribe one.
- Use pharmacy discount apps like GoodRx - they often beat insurance prices.
- Buy 90-day supplies when possible. Many pharmacies charge the same for 30 or 90 days.
- Know your PBM. Some insurers have better generic coverage than others.
If you’re in Europe:
- Ask your pharmacist if substitution is allowed - you might save money.
- Compare prices between pharmacies. In Germany and France, prices can vary by 20%.
- Don’t assume your country’s price is the lowest. A 2025 study showed some U.S. generics were cheaper than European ones, even after currency conversion.
Why This Matters Beyond Your Prescription
This isn’t just about pills. It’s about how societies value health, innovation, and fairness. The U.S. system rewards competition and speed. Europe rewards control and equity. Both have trade-offs. And the world is watching. As drug costs rise everywhere, countries are trying to copy each other. The U.S. is looking at reference pricing. Europe is wondering if it can afford to keep underpaying for innovation.
One thing’s clear: the old model won’t last. Generic prices in the U.S. won’t stay this low forever. Brand-name prices in Europe won’t stay this low either. The real question isn’t who pays more - it’s who gets to decide what’s fair.


Donny Airlangga
7 01 26 / 22:05 PMMan, I never thought about it this way - we pay insane prices for new drugs so the world can get cheap generics. Kinda wild when you put it like that.
Prakash Sharma
7 01 26 / 22:48 PMUSA still rules. You think Europe’s ‘fair’? They ride on our R&D like parasites and then act like they’re morally superior. We make the pills, they whine about the cost. Pathetic.
swati Thounaojam
9 01 26 / 08:57 AMgeneric lisinopril for $4?? i need this in india too
Aubrey Mallory
9 01 26 / 22:46 PMLet’s be real - if we didn’t have PBMs squeezing suppliers, we wouldn’t have $4 generics. The system’s broken, but it works for people who know how to game it. GoodRx, 90-day fills, and asking for the cash price? That’s how you survive.
And yeah, the shortages? That’s the cost of pricing drugs like toilet paper. No one invests in quality when they’re barely scraping by.
Dave Old-Wolf
11 01 26 / 02:14 AMSo if the U.S. pays more for brand names, and Europe pays more for generics, who’s actually getting the better deal? Like… if I’m on metformin, I’m golden. But if I need a new cancer drug, I’m screwed. Is that fair? Feels like we’re trading one kind of pain for another.
Ken Porter
12 01 26 / 20:33 PMEuropeans pay more for generics? LMAO. They can’t even handle a competitive market. They want everything handed to them on a silver platter while blaming America for their own lack of innovation.
Manish Kumar
13 01 26 / 03:47 AMThink about it - this isn’t about drugs. It’s about the soul of capitalism versus the ghost of socialism. The U.S. says: ‘If you want to innovate, you pay for it.’ Europe says: ‘Let’s all share the cost, but don’t expect to get it fast.’ One system feeds the future. The other just redistributes the past. Which one do you want to live in? The one that builds, or the one that just waits?
And don’t tell me ‘fairness.’ Fairness is a myth. The market doesn’t care about your feelings. It cares about who’s willing to pay the price of progress.
So yes, we pay more. But we’re the ones who made Wegovy. We’re the ones who developed mRNA vaccines in a year. Europe got the benefit. We got the burden. And honestly? I’d do it again.
Molly Silvernale
13 01 26 / 05:22 AMIt’s like… the U.S. is the wild west pharmacy - guns blazing, prices crashing, shortages popping up like weeds - but somehow, you walk out with a $2 bottle of ibuprofen and a side of existential dread. Meanwhile, Europe’s pharmacy is a quiet, orderly library with a librarian who says, ‘I’m sorry, but this medication is only approved for patients over 55 with a referral from a priest.’
We’re not better. We’re just louder. And we’re the ones who paid for the library’s entire collection - then got kicked out because we yelled too loud while browsing.
Kristina Felixita
13 01 26 / 08:02 AMAs someone who moved from the U.S. to Germany - I used to get my blood pressure meds for $4. Now I pay €12 for the same thing. But when my mom got her new cancer drug? Covered. No copay. No paperwork. No GoodRx app needed. I miss the $4 pills… but I’d trade them for peace of mind any day.
It’s not about who’s right. It’s about what kind of society you want to be.
Joanna Brancewicz
13 01 26 / 12:17 PMThe PBM rebate structure creates perverse incentives: manufacturers inflate list prices to maximize rebates, while patients pay the inflated co-pay. Net-net, the system extracts value without transparency. It’s a classic principal-agent problem with insulin.
Evan Smith
15 01 26 / 07:13 AMSo… we pay more so Europe can sleep at night? Cool. So when I’m broke and my insulin costs $500, I’m basically funding someone else’s ‘fair’ healthcare? Thanks, America. Real noble.
Lois Li
16 01 26 / 18:04 PMThat comment about funding innovation… I get it. But what if we could do both? What if we didn’t have to choose between crushing people with bills and letting people die waiting? Maybe we’re just not trying hard enough to fix it.
christy lianto
17 01 26 / 04:14 AMDon’t let them fool you - this isn’t about ‘fairness.’ It’s about power. The U.S. holds the cards because we’re the only ones with the cash to gamble on unproven science. Europe plays it safe. But safe doesn’t save lives. Bold does.
And yes - the shortages? That’s the cost of greed. But don’t blame the system. Blame the companies that stopped making pills because they couldn’t make a 500% profit on a $0.01 pill.
Luke Crump
18 01 26 / 06:47 AMWait - you’re telling me the U.S. is the *cheapest* for generics? That’s not a feature, that’s a BUG. A broken market isn’t a victory. It’s a collapse. If you can’t make a profit, you don’t make the drug. If you don’t make the drug, people die. That’s not efficiency - that’s a death spiral disguised as a deal.
Annette Robinson
18 01 26 / 20:25 PMThank you for this balanced breakdown. It’s rare to see the full picture - not just the outrage, but the trade-offs. The U.S. system is messy, but it’s the engine. Europe’s is calm, but it’s a passenger. We need both - and we need to fix the parts that hurt real people.