When you're on a blood thinner like apixaban, rivaroxaban, or dabigatran, even a simple change in your medication routine can have serious consequences. These drugs - known as DOACs (Direct Oral Anticoagulants) - are meant to prevent clots without the constant blood tests that warfarin requires. But they’re not foolproof. Many patients take five or more other medications, and that’s where things get risky.
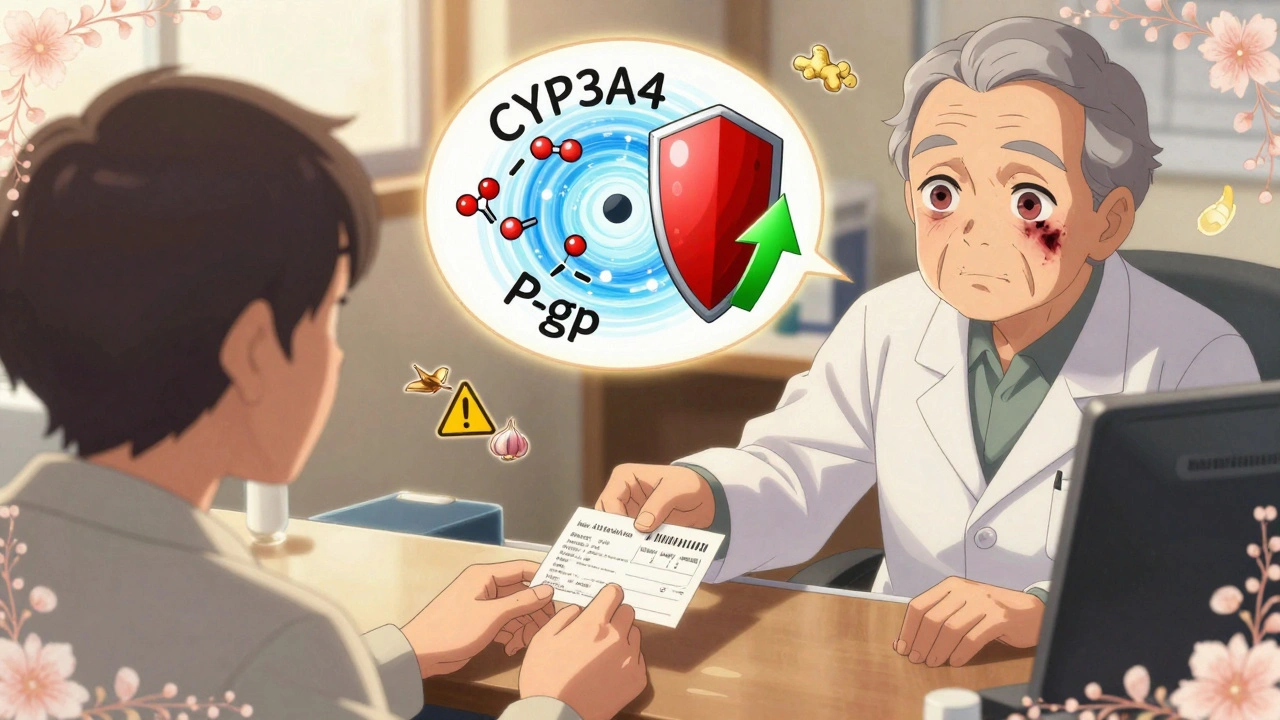
DOACs work by blocking specific proteins in your blood to stop clots from forming. But their effectiveness depends on how much of the drug stays in your system - and that’s easily disrupted by other medicines. Unlike warfarin, which reacts with vitamin K in food, DOACs are mostly affected by how your body absorbs and breaks them down. Two key systems control this: the CYP3A4 enzyme and the P-gp transporter. Many common drugs mess with one or both.
If you take something that blocks CYP3A4 or P-gp, your DOAC levels can spike. That means more bleeding risk - bruising, nosebleeds, even internal bleeding. If you take something that speeds up these systems, your DOAC levels can drop. That’s when clots form - stroke, heart attack, deep vein thrombosis. It’s not theoretical. Studies show unrecognized drug interactions are a leading cause of DOAC-related complications.
Not all DOACs react the same way. Here’s how they compare:
That’s why you can’t treat them like interchangeable pills. A drug that’s safe with apixaban might be dangerous with dabigatran.
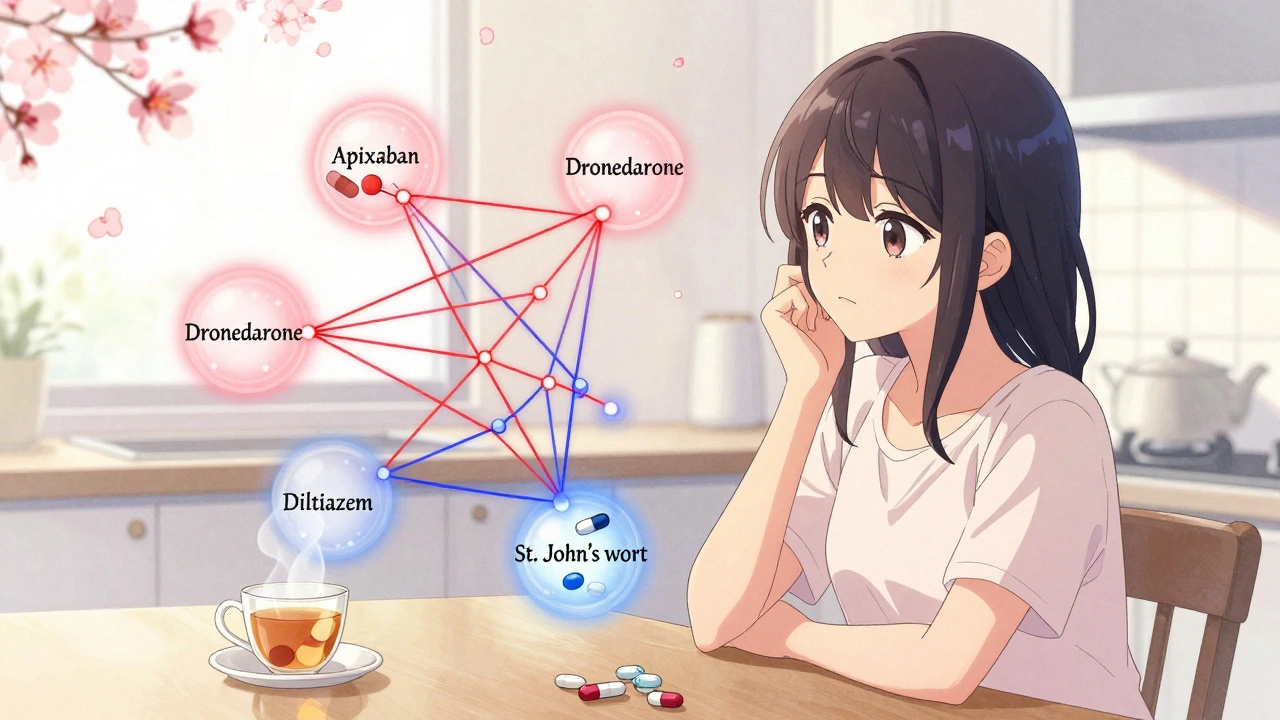
These aren’t obscure drugs - they’re prescribed to millions. Here’s what to watch for:
Even over-the-counter meds can be risky. Some herbal supplements - like ginseng, garlic, or ginger - can thin your blood too. They don’t change DOAC levels, but they add to the bleeding risk. Same with NSAIDs like ibuprofen or naproxen. If you need pain relief, acetaminophen is safer.
You might be on aspirin, clopidogrel, or an SSRI like sertraline. These don’t change how your body handles DOACs. But they make your blood thinner in a different way. Add them together, and your bleeding risk doesn’t just go up - it multiplies.
Studies show that combining DOACs with SSRIs or NSAIDs increases the chance of stomach bleeding by 2-3 times. That’s why doctors now ask: Is this combo truly necessary? If you have arthritis and take naproxen daily, can you switch to physical therapy? If you’re on antidepressants, is there a non-bleeding-risk option?
There’s no blanket rule. It’s about weighing benefits. For someone with a history of heart attack, aspirin + DOAC might be worth the risk. For an older person with mild depression, skipping the SSRI might be safer.
Most DOACs are cleared by the kidneys. If your kidney function drops - and it often does with age or diabetes - your DOAC builds up. That’s why lower doses are used in people with reduced kidney function.
Now imagine you’re on a DOAC, have mild kidney impairment, and start taking diltiazem. Your kidneys are already struggling to clear the drug. Diltiazem slows down its breakdown. The result? A double hit. Your DOAC level could jump dangerously high.
Doctors don’t just check your DOAC dose. They check your eGFR (kidney function number). If it’s below 50 mL/min, even a "safe" interaction can become dangerous. Always tell your pharmacist and doctor your latest kidney test results.
You don’t need to memorize every interaction. But you do need a system:
Right now, we rely on guidelines based on limited studies. But researchers are pushing for more. Some are testing whether we can measure DOAC levels in the blood to adjust doses - like we do with warfarin. It’s not standard yet. But it might be soon.
Also, new drugs are coming. Cancer treatments, antivirals, even some weight-loss pills can affect CYP3A4 or P-gp. The list of risky combinations keeps growing. That’s why education is critical. Many doctors still think DOACs are "safe" and don’t check interactions closely enough.
The truth? DOACs are easier than warfarin - but not risk-free. Their advantage isn’t that they don’t interact. It’s that the interactions are more predictable. Once you know which ones to watch for, you can manage them.
If you’re on a DOAC, you’re not just taking one drug. You’re managing a system. Every new pill, every change in kidney function, every supplement - it all matters. The best thing you can do is stay informed and speak up.
Ask your doctor: "Which of my meds could interfere with my blood thinner?" Ask your pharmacist: "Is this new prescription safe with apixaban?" And if you’re ever unsure - wait. Don’t take it until you have a clear answer.
Bleeding and clotting aren’t just side effects. They’re life-threatening outcomes - and many are preventable.
Jack Arscott
2 12 25 / 00:37 AMJust got prescribed apixaban last week and I was already panic-scrolling through every med I take 😅
Turns out my turmeric supplement is on the list… guess I’m switching to curry powder instead. Thanks for the checklist - saved my life (probably).
Walker Alvey
3 12 25 / 19:36 PMOh wow another article telling us we’re all gonna die if we take a pill that isn’t in the 0.003% approved list
Meanwhile my grandma takes aspirin, garlic, and three different teas and still walks 5 miles a day
Maybe the real problem is doctors who treat patients like lab rats instead of humans
Adrian Barnes
4 12 25 / 19:52 PMIt is not merely a matter of pharmacokinetic interaction; it is a systemic failure of clinical vigilance. The conflation of convenience with safety has precipitated a public health crisis of iatrogenic origin. The proliferation of DOACs, while ostensibly streamlining anticoagulation therapy, has engendered a dangerous illusion of benignity. Patients are not being educated; they are being deployed. The CYP3A4/P-gp axis is not a footnote - it is the fulcrum upon which life and death balance. To disregard this is not negligence - it is epistemic arrogance.
Jaswinder Singh
5 12 25 / 07:15 AMBro this is fire. I’m a nurse in Mumbai and I see this every damn day. Old people on 8 meds, no one checks interactions. One guy took St. John’s wort with rivaroxaban and ended up in ICU with a brain bleed. No one told him it was dangerous. This post? It’s a goddamn lifeline. Share it with your grandma.
Bee Floyd
7 12 25 / 00:51 AMThere’s something beautiful about how a tiny pill can hold so much power - and how easily we forget that. I used to think ‘blood thinner’ meant ‘don’t cut yourself’… turns out it’s more like ‘don’t breathe wrong around certain herbs’. I keep a laminated card in my wallet now: DOAC + meds + kidney number. Feels weird to carry it, but way less weird than ending up in the ER because I took ibuprofen for a headache. Thanks for making this feel less scary and more manageable.
Jeremy Butler
8 12 25 / 13:18 PMThe notion that DOACs are inherently safer than warfarin is a misinterpretation of pharmacological simplicity. The absence of dietary restrictions and routine INR monitoring does not equate to reduced complexity. Rather, the burden of cognitive load is transferred from the clinician to the patient, often without adequate support infrastructure. The resultant clinical vulnerability is not a function of drug design, but of sociomedical neglect.
Courtney Co
9 12 25 / 19:34 PMWait so you’re telling me my 78-year-old dad can’t take his ginger tea anymore? Or his fish oil? Or his vitamin E? What’s next? Are we gonna ban sunlight because it might make his blood thinner? I mean… I get it, but this feels like fear-mongering dressed up as science. Who even decides what’s ‘dangerous’? The FDA? A guy in a lab coat who’s never met a real patient? I’m just saying - maybe we should trust people more and scare them less.
Shashank Vira
9 12 25 / 22:52 PMHow quaint. You speak of ‘checklists’ and ‘pharmacists’ as if these are universally accessible institutions. In the Global South, where I practice, patients choose between food and medicine - let alone a pharmacist who knows CYP3A4 from P-gp. This article reads like a luxury pamphlet for the privileged. The real tragedy isn’t the interaction - it’s the system that lets this knowledge remain a privilege, not a right.