
Every year, over 80% of American adults reach for an over-the-counter (OTC) medication before calling their doctor. Whether it’s a headache, stuffy nose, or upset stomach, these pills and liquids are right there on the shelf-no appointment needed. But just because you don’t need a prescription doesn’t mean they’re harmless. Many people treat OTC drugs like candy, popping extra tablets or mixing them without realizing the risks. The truth is, OTC medications can cause serious harm if used wrong-and far too often, they do.
OTC medications are drugs approved by the FDA for safe use without a doctor’s order. They’re meant for short-term relief of minor, self-diagnosable conditions like pain, fever, allergies, heartburn, or coughs. There are more than 100,000 different OTC products on the market in the U.S., made from around 800 active ingredients. These aren’t just pills-some are nasal sprays, creams, eye drops, even toothpastes with fluoride. The key is they’re designed to be safe when used as directed, but dangerous when misused.
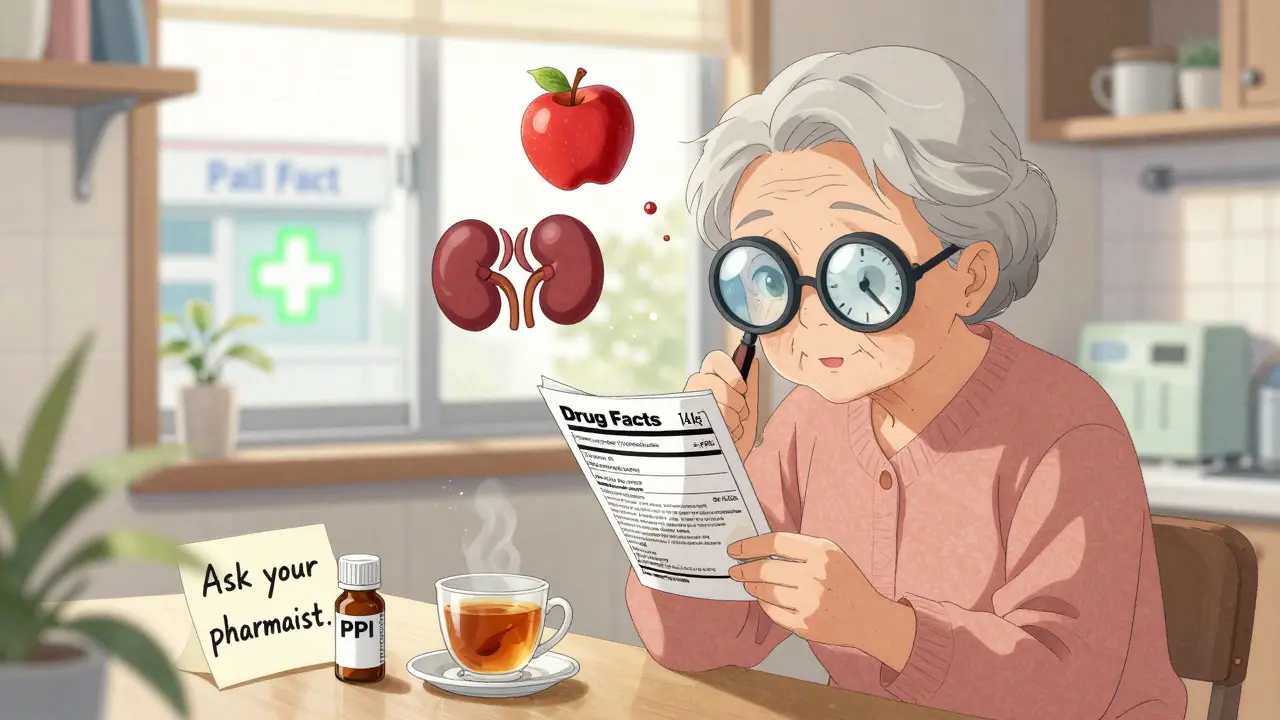
The modern system started in the 1930s, but it wasn’t until the 1950s that the line between prescription and OTC became clear. Today, every OTC product must have a standardized Drug Facts label. This label tells you exactly what’s in it, how to use it, what to watch out for, and when to stop. If you don’t read this label, you’re guessing-and guessing with medicine is risky.
If you’ve ever taken Tylenol or Advil, you’ve used one of the most common OTC categories: pain relievers. But they’re not the same. Acetaminophen (Tylenol) and NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) work differently and carry different risks.
Acetaminophen is great for reducing fever and easing mild to moderate pain. It’s often the go-to for kids, pregnant women, and people with stomach issues because it doesn’t irritate the gut like NSAIDs do. But here’s the catch: it can wreck your liver. The FDA says more than 15,000 people end up in the hospital every year from acetaminophen overdose. The maximum daily dose is 4,000 mg-but that’s easy to hit if you’re taking multiple products. Cold medicines? Pain patches? Some contain acetaminophen too. You might not realize you’re doubling up.
NSAIDs, on the other hand, reduce inflammation. That makes them better for sprains, arthritis, or menstrual cramps. But they can cause stomach bleeding, especially if you take them daily or on an empty stomach. People with ulcers, kidney disease, or high blood pressure should avoid them. And if you’re over 60, your risk goes up. A 2021 study found NSAIDs increase gastrointestinal bleeding risk by 2 to 4 times.
Bottom line: Use acetaminophen if you’re worried about your stomach. Use NSAIDs if you need inflammation control. Never take more than directed. And always check other meds you’re taking-they might already have one of these ingredients.
When you’ve got a runny nose or itchy eyes, OTC cold and allergy meds can feel like a lifesaver. But many of them are overkill-or worse, dangerous.
Pseudoephedrine (Sudafed) is a nasal decongestant that works well, but it’s kept behind the pharmacy counter because it can be used to make illegal drugs. You need to show ID and sign a log. Dextromethorphan (found in Robitussin, Delsym) suppresses coughs, but teens have abused it for its hallucinogenic effects. More than 1.2 million ER visits a year are linked to OTC drug misuse, and dextromethorphan is a top offender.
Then there’s guaifenesin (Mucinex), an expectorant that helps thin mucus. It doesn’t cure your cold, but it can make you feel less stuffed up. For allergies, you’ve got two main choices: first-generation antihistamines like diphenhydramine (Benadryl) and second-generation ones like loratadine (Claritin) and fexofenadine (Allegra).
Diphenhydramine makes you sleepy-so much so that the FAA bans pilots from flying within 12 hours of taking it. It also increases fall risk in older adults by 30%. If you’re over 65, don’t use it for sleep. Loratadine and fexofenadine don’t cause drowsiness in most people and last longer. They’re safer for daily use and better for driving or working.

Heartburn is common, and OTC meds like Tums, Pepcid, and Prilosec are everywhere. But using them long-term can backfire.
Antacids like calcium carbonate (Tums) give quick relief by neutralizing acid. They’re fine for occasional use. H2 blockers like famotidine (Pepcid AC) reduce acid production and last longer. But proton pump inhibitors (PPIs) like omeprazole (Prilosec OTC) are the strongest-and the riskiest. A 2023 study in JAMA Internal Medicine found that using PPIs for more than a year increases your risk of chronic kidney disease by 20-50%. They’re meant for short-term use (14 days at a time), not daily for months or years.
And don’t forget loperamide (Imodium). It stops diarrhea fast, but if you take too much, it can cause dangerous heart rhythms. People with kidney problems need to be careful with the dose. Also, if diarrhea lasts more than two days, see a doctor-it could be something serious like an infection.
Not everyone can safely use OTC drugs. Certain groups need extra caution-or should avoid them entirely.
During pregnancy, acetaminophen is the only recommended pain reliever. NSAIDs like ibuprofen can harm fetal kidneys after 20 weeks. For kids under 4, cough and cold medicines are banned because of past deaths from overdose. For older adults, diphenhydramine increases fall risk and confusion. If you have liver disease, avoid acetaminophen. If you have kidney disease, avoid NSAIDs and loperamide. If you have diabetes, check sugar content in liquid syrups.
Even something as simple as an antacid can interfere with other meds. Calcium carbonate can block absorption of antibiotics like tetracycline. Always ask your pharmacist if your OTC medicine will react with your prescriptions.
Here’s how to avoid the most common mistakes:
And if symptoms don’t improve in a few days-or get worse-stop the OTC medicine and see a doctor. These aren’t cures. They’re temporary fixes.
OTC meds are for minor, short-term issues. If you need them for more than a week, something else might be going on. Here’s when to get help:
Many people delay seeing a doctor because they think OTC meds should fix everything. But ignoring symptoms can turn a small problem into a big one.
OTC meds are changing. CVS now has an AI app that checks your meds and warns you about interactions. Pharmacists in some states can now prescribe certain OTC drugs directly-no doctor needed. That’s a good thing, because people need more guidance, not less.
But the biggest challenge remains: people still think OTC means risk-free. It doesn’t. The FDA says 25% of adults believe OTC drugs are always safe, no matter how much they take. That’s why accidental overdoses are so common. The solution isn’t more drugs-it’s better education.
Next time you pick up an OTC product, pause. Read the label. Ask yourself: Is this really what I need? Could this hurt me? Am I using it for the right reason? Your health isn’t a guessing game.
Yes, you can take them together if needed-for example, if one alone isn’t controlling your pain. They work differently, so combining them can be more effective. But stick to the recommended doses for each. Don’t exceed 4,000 mg of acetaminophen per day or 1,200 mg of ibuprofen. Avoid long-term daily use unless directed by a doctor.
Second-generation antihistamines like loratadine (Claritin) and fexofenadine (Allegra) are generally safe for daily use. They don’t cause drowsiness and are designed for ongoing symptom control. But if you’re using them for more than a few weeks without relief, see a doctor. You might need a different treatment, like a nasal steroid spray, or have an underlying condition like sinusitis.
The FDA banned cough and cold medicines for children under 4 because they caused serious side effects-including seizures, rapid heart rate, and death-in young kids. Their bodies process these drugs differently, and even small doses can be toxic. For kids under 4, use saline drops, a humidifier, and honey (for children over 1) to ease coughs. Always check with your pediatrician first.
Acetaminophen is considered the safest option for pain and fever during pregnancy. NSAIDs like ibuprofen and naproxen should be avoided, especially after 20 weeks, because they can affect fetal kidney development and reduce amniotic fluid. Always check with your OB-GYN before taking any OTC medicine-even if it’s labeled "safe."
Most expired OTC meds lose potency over time, meaning they won’t work as well. They rarely become dangerous, but some-like liquid antibiotics or eye drops-can grow bacteria after expiration. For pain relievers or antihistamines, using them past the date is usually low risk but not effective. When in doubt, throw them out. Many pharmacies offer take-back programs for expired meds.
Palesa Makuru
3 01 26 / 03:25 AMUgh, I can't believe people still think OTC means 'free for all'. I had a neighbor take 12 Tylenol because she 'felt like it' and ended up in the ER. Like, ma'am, you don't get to treat your liver like a disposable napkin.
Lori Jackson
4 01 26 / 04:41 AMIt's not just misuse-it's systemic pharmacological illiteracy. The FDA's Drug Facts label is a masterclass in harm reduction, yet 78% of consumers skip it entirely. This isn't negligence; it's epistemic arrogance wrapped in Advil bottles.
Wren Hamley
4 01 26 / 18:46 PMWait-so if I take Aleve for my knee and NyQuil for my cold, I'm basically doing a slow-mo liver demolition derby? 🤯 I thought NyQuil was just for sleep. Turns out it's also a surprise acetaminophen party. No wonder my grandma's liver enzymes looked like a stock market crash.
veronica guillen giles
5 01 26 / 10:49 AMOh honey, you think that’s bad? I had a cousin take 3 days of Imodium because she didn’t want to leave the house during her period. Got admitted for torsades de pointes. She’s fine now. But now she calls herself ‘the queen of constipation’. 🤦♀️
Ian Ring
7 01 26 / 05:02 AMSo true. I always check labels. Always. And I ask the pharmacist. Always. Even if I'm just buying cough drops. They know more than your Google search. Seriously. I've saved myself from three drug interactions just by saying 'Hi, can you check this?'
Tru Vista
8 01 26 / 19:45 PMOTC = OverTrusted Crap. Just say it. Stop pretending it’s safe. People die from this. Every. Single. Day.
Tiffany Channell
9 01 26 / 08:38 AMOf course you’re not supposed to mix meds. But you know who does? The people who don’t read the label. And they’re the same people who think ‘natural’ means ‘safe’. Like, no. Dandelion tea won’t fix your pancreas. And yes, I’ve seen it happen.
Joy F
11 01 26 / 06:44 AMLet’s be real: OTC meds are capitalism’s way of outsourcing medical responsibility to the masses. We’re not just consumers-we’re unpaid pharmacists, self-diagnosing with TikTok and desperation. And the system? It loves it. More pills sold. Less doctors needed. Less liability. It’s genius. If you’re a corporation.
Haley Parizo
12 01 26 / 02:57 AMThis isn’t about pills. It’s about how we’ve lost trust in our bodies. We don’t sit with pain anymore. We don’t rest. We don’t drink tea. We don’t breathe. We just reach for the bottle because we’ve been taught that discomfort is an error to be corrected-not a signal. The real crisis isn’t acetaminophen. It’s our relationship with suffering.
Ian Detrick
13 01 26 / 11:17 AMLook, I get it. Life’s busy. But if you’re popping pills like Skittles, maybe slow down. Take a walk. Drink water. Sleep. Sometimes the best medicine isn’t on the shelf-it’s in your bedroom, your kitchen, or your quiet corner. Just saying.
Angela Fisher
14 01 26 / 12:57 PMDid you know the FDA gets pressure from Big Pharma to keep certain drugs OTC? Like, they don’t want to lose the cash flow. And the labels? They’re written by lawyers, not doctors. That’s why they’re so confusing. And don’t get me started on how they hide the real risks in tiny print. It’s all a scam. They want you addicted. They want you dependent. They want you buying more next month.
Neela Sharma
16 01 26 / 11:52 AMIn India, we call this 'dawa ka jadoo'-medicine magic. People buy 10 different cough syrups at once and mix them like cocktails. My aunty took 3 types of antacids with her blood pressure pill and ended up in the hospital. We laughed. Then we cried. Then we bought her a big poster of the Drug Facts label. Now it hangs above her fridge. Like a prayer.
Sarah Little
16 01 26 / 17:48 PMJust a note: many people don’t know that 'sugar-free' doesn't mean 'safe for diabetics'-some OTC syrups have hidden carbs or artificial sweeteners that spike glucose. Always check the inactive ingredients. I’ve seen this ruin HbA1c levels. Just saying.
innocent massawe
17 01 26 / 07:28 AMMy cousin in Lagos takes paracetamol for everything-headache, fever, even stress. He says, 'It’s just a pill, bro.' I told him, 'Bro, your liver doesn’t care if you’re stressed or not.' He laughed. Then he stopped. For a week. Progress.
erica yabut
18 01 26 / 08:28 AMIt’s not just the meds-it’s the packaging. Bright colors. Bold fonts. ‘Fast Relief!’ ‘Works in Minutes!’ It’s designed to trigger dopamine. We’re not just buying medicine-we’re buying emotional relief disguised as science. And the companies know it. They’re not selling pills. They’re selling hope. And hope? That’s the most profitable drug of all.