
Chemotherapy isn’t just one drug-it’s a whole system of powerful chemicals designed to attack cancer by targeting cells that divide fast. It’s been around since the 1940s, when scientists first noticed that mustard gas exposure in WWII soldiers led to a drop in white blood cells. That observation led to the first chemotherapy drug, nitrogen mustard, used on a patient with lymphoma in 1942. Today, over 100 different chemotherapy drugs are in use, each with its own way of disrupting cancer cells. But here’s the catch: they don’t just hit cancer. They hit any fast-dividing cell in your body. That’s why side effects happen.
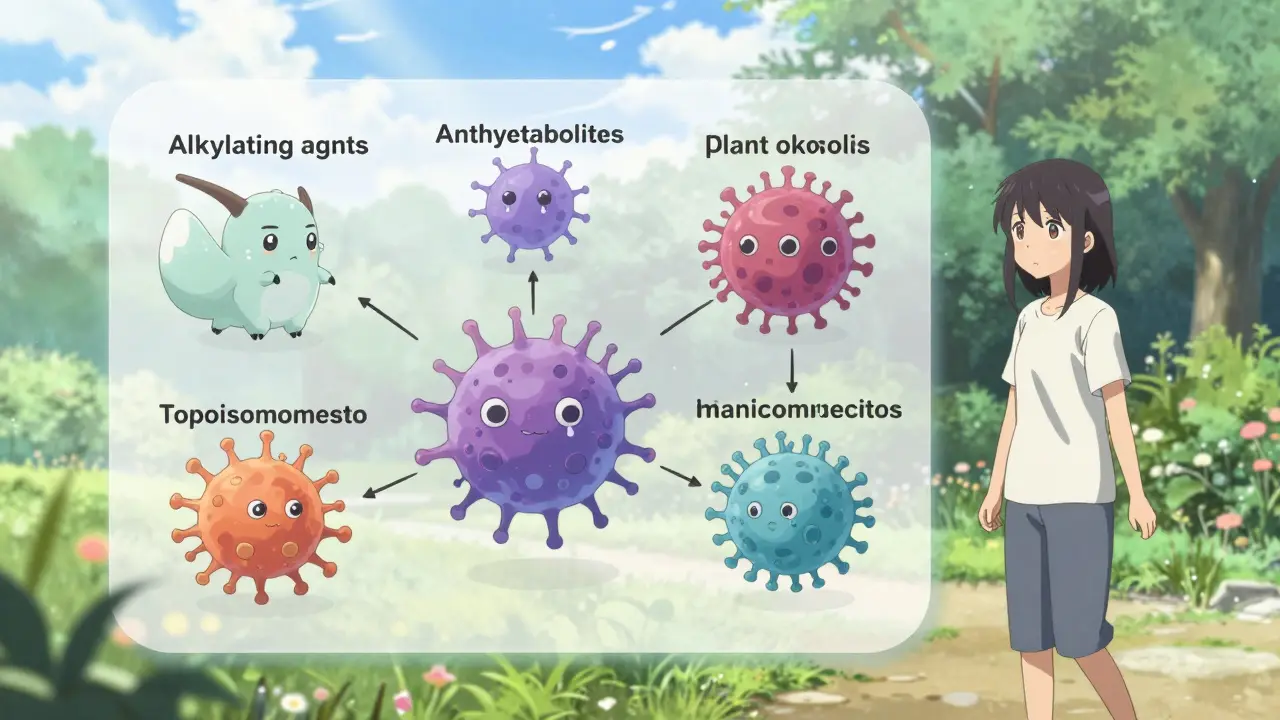
Chemotherapy works because cancer cells grow and divide much faster than most normal cells. That’s their weakness-and also the reason these drugs can be so damaging to healthy tissue. There are six main classes of chemotherapy drugs, each attacking cancer in a different way.
These drugs are chosen based on the type of cancer, how advanced it is, and even genetic markers in the tumor. For example, paclitaxel is commonly used in breast cancer at a dose of 175 mg per square meter of body surface every three weeks. Oral drugs like capecitabine are taken twice daily for two weeks, then paused for a week to let the body recover.
Most chemotherapy is given through an IV-about 65% of the time. But some are pills, injections into the spinal fluid, or even delivered directly into the abdomen or arteries. The treatment isn’t continuous. It’s given in cycles: a few days of treatment, then rest. This lets healthy cells bounce back while keeping pressure on the cancer.
You might hear that targeted therapies and immunotherapies are replacing chemotherapy. And yes, in some cancers, they are. But chemotherapy hasn’t been phased out-it’s been refined.
For cancers like acute myeloid leukemia (AML) and diffuse large B-cell lymphoma, chemotherapy is still the first-line treatment for over 75% of patients. In ovarian cancer, nearly all patients get chemo. For colorectal cancer, it’s used in 85% of cases. Even in breast cancer, where targeted drugs like Herceptin are common, chemo is still given before surgery in many cases to shrink tumors. Studies show that when chemo gets rid of all visible cancer after surgery (called a pathologic complete response), survival rates jump.
Chemotherapy also has unique strengths. It can cross the blood-brain barrier, making it one of the few treatments that can reach brain tumors. It works on tumors with many different cell types, unlike targeted drugs that only hit one specific mutation. And it starts working within hours-something immunotherapy can’t always do.
Still, it’s not perfect. Some cancers, like slow-growing prostate cancer, respond better to hormone therapy than chemo. And resistance can develop-cancer cells learn to pump drugs out using proteins like P-glycoprotein. That’s why chemo is often combined now: with targeted drugs, immunotherapies, or radiation.
Back in the 1980s, vomiting after chemo was almost guaranteed. Today, it’s not. That’s because of drugs like ondansetron, which block the signals that trigger nausea. In the past, 70-80% of patients on strong chemo regimens had severe vomiting. Now, it’s down to 10-20%.
But other side effects still stick around-and some are worse than you’d expect.
One surprising finding? Hydration matters. Drinking 1-2 liters of water daily reduces fatigue and prevents kidney damage from some drugs. Eating small, bland meals-toast, rice, bananas-helps more than big meals when nausea strikes.
It’s not just about drugs. Lifestyle changes make a big difference.
Most patients learn what works for them by the third cycle. It’s trial and error. What helps one person might not help another. Keep talking to your care team. They’ve seen it all.
The field isn’t standing still. In June 2023, the FDA approved trilaciclib (Cosela), the first drug designed to protect bone marrow during chemo. It’s used in lung cancer patients to reduce the chance of low blood counts-a major cause of treatment delays.
Scalp cooling is becoming more common. A 2022 study showed it cuts hair loss from 65% to 25% in breast cancer patients on taxanes. More clinics are offering it.
Cannabis-based treatments are being studied. One 2023 study found CBD and THC combinations reduced neuropathic pain by 55%. While not yet standard, it’s a growing area of research.
And here’s the truth: chemotherapy won’t disappear. Even with all the new drugs, it’s still needed for cancers without clear targets. Experts say it will remain essential for at least the next 20 years. But it’s changing-less about brute force, more about smart combinations and better support.
On forums and surveys, patients consistently say:
They also praise the support teams-the nurses who check in between cycles, the nutritionists who help with appetite, the counselors who listen when it all feels too heavy.
Yes. When targeted therapies stop working-often because the cancer mutates-chemotherapy is frequently the next step. It doesn’t rely on specific mutations, so it can still kill cancer cells that have escaped other treatments. Many patients receive chemo after targeted drugs fail, especially in cancers like lung, breast, and colon.
It can do both. In some cancers-like testicular cancer, Hodgkin lymphoma, and certain leukemias-chemotherapy can cure the disease. In others, like advanced lung or pancreatic cancer, it’s used to shrink tumors, slow growth, and extend life with better quality. The goal depends on the cancer type, stage, and individual health.
It depends on the drug. Alkylating agents and anthracyclines are more likely to cause hair loss than antimetabolites. Some people have genetic differences that make their hair follicles more sensitive. Scalp cooling can help, but it’s not 100% effective for everyone. Also, hair loss is usually temporary-hair usually grows back after treatment ends.
No. Chemotherapy temporarily lowers white blood cell counts, especially neutrophils, which fight infection. But bone marrow usually recovers after each cycle. Most people’s immune systems return to normal within months after treatment ends. Long-term immune suppression is rare unless chemo was given for years or combined with radiation.
Some are safe, others aren’t. Antioxidants like high-dose vitamin C or E might interfere with how chemo kills cancer cells. Vitamin D is recommended for people on taxanes if levels are low, since deficiency may worsen nerve damage. But don’t take supplements without talking to your oncologist. What’s safe for one person might be risky for another.
Chemotherapy is harsh. It’s not glamorous. It doesn’t feel fair. But for millions of people, it’s the difference between life and death. It’s not the future of cancer care-but right now, it’s still the backbone. The real progress isn’t in replacing it. It’s in making it smarter: better timing, fewer side effects, smarter combinations, and more support. The goal isn’t just to kill cancer. It’s to help you live through it.
Leave a comments