
ALS, or amyotrophic lateral sclerosis, isn’t just muscle weakness. It’s the slow, silent death of the nerves that tell your muscles to move. These nerves-called motor neurons-start in your brain, run down your spinal cord, and connect to every muscle you use to walk, talk, swallow, or even breathe. When they die, the signals stop. Muscles shrink. Paralysis sets in. Most people live only 3 to 5 years after symptoms begin. There’s no cure. No reversal. Just slowing the fall.
This isn’t a mystery you can fix with vitamins or exercise. It’s a biological breakdown. About 90% of cases happen without a family history. The other 10% are genetic. But no matter the cause, the end result is the same: your body becomes a prison you can’t escape. And until recently, doctors had nothing to offer but sympathy.
In 1995, after decades of failed experiments, the FDA approved riluzole. It wasn’t a miracle. It didn’t bring back movement. It didn’t stop ALS. But for the first time, it gave patients a fighting chance-just a few extra months.
Riluzole is a small molecule, a benzothiazole compound with a molecular weight of 235.23 g/mol. It doesn’t cure ALS, but it interferes with the process that kills motor neurons. The leading theory? Glutamate excitotoxicity. Glutamate is a natural brain chemical that tells neurons to fire. But in ALS, too much of it builds up. It overstimulates nerve cells until they burn out. Riluzole blocks this overload. It reduces glutamate release, shuts down sodium channels on nerve terminals, and dampens the signals that lead to cell death.
It’s not perfect. Scientists still don’t fully understand how it works. Other drugs that target glutamate failed. But riluzole stuck. And for 22 years, it was the only FDA-approved drug for ALS.
Let’s talk numbers. In the landmark 1996 Lancet trial, 959 patients were given either placebo or riluzole at 50mg, 100mg, or 200mg daily. At 18 months, those on 100mg daily had a 35% lower risk of death or needing a tracheostomy than those on placebo. That’s the number doctors cite. But what does it mean in real life?
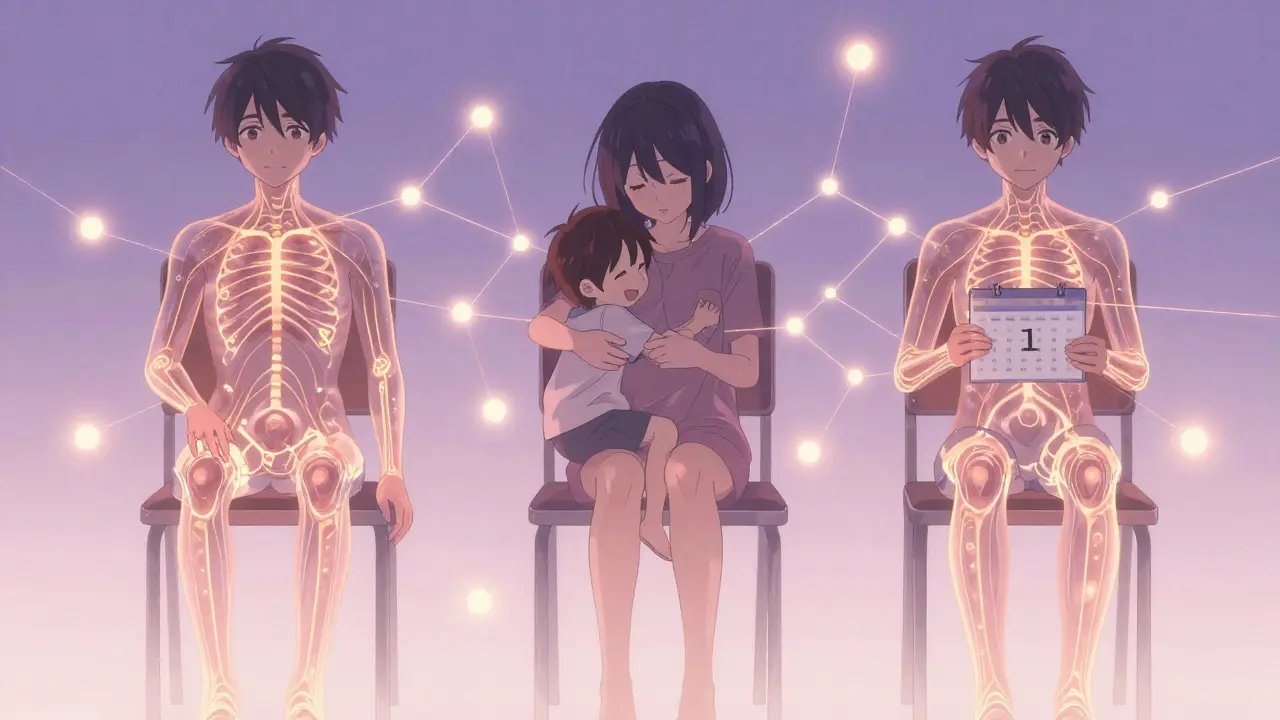
On average, riluzole extends survival by 2 to 3 months. For some, it’s longer. For others, barely noticeable. But in a disease that kills so fast, even one extra month matters. One more birthday. One more hug. One more conversation.
Real-world data is messier. Some studies show 6 to 19 months of extended life. Others show no benefit at all. Why the difference? Because ALS doesn’t move the same way in everyone. Some decline slowly. Others crash. Riluzole works better for those with slower progression. It’s not a one-size-fits-all fix.

Riluzole comes in three forms: tablets (Rilutek), oral suspension (Tiglutik), and an oral thin film (Exservan). The standard dose is 50mg twice a day-100mg total. You take it on an empty stomach, one hour before or two hours after meals. Absorption is about 60%, and it peaks in your blood within 90 minutes. Half-life? 7 to 15 hours. That’s why you can’t just take it once a day.
The thin film version, approved in 2020, is designed for people who have trouble swallowing. It dissolves on the tongue. One study showed 30% fewer stomach issues compared to tablets. That’s huge for someone already struggling with eating.
Cost varies. In the U.S., brand-name riluzole can run $1,000 a month. Generic versions are cheaper, but not always available. Globally, access is uneven. In low-income countries, only 15-20% of patients can afford it without help. That’s not just a medical issue-it’s a justice issue.
Nothing comes without a price. Riluzole’s side effects are real-and for some, worse than the disease.
That last one is serious. Your liver has to process riluzole. If it’s already stressed, things can go wrong. Doctors require liver function tests before you start-and monthly for the first three months. If enzymes climb too high, you stop. One Reddit user wrote: “After 9 months, my liver was 3x normal. I had to quit. Frustrating when the only drug that might help damages your liver.”
Drug interactions matter too. Caffeine slows riluzole clearance. Theophylline (used for asthma) can spike to dangerous levels when taken with riluzole. People on these meds need careful monitoring.
Eight out of ten newly diagnosed ALS patients start riluzole. That’s the standard. But adherence drops fast. By 12 months, only 63% are still taking it. At 24 months? Just 47%.
Why? Side effects. Cost. Hope fading. A 2022 survey of 2,845 patients found that 8% quit because side effects were unbearable. Others stopped because they felt it wasn’t working. But here’s the twist: 62% of those who stayed on it said they believed it gave them extra time. And 43% of those said it was for “more time with family.”
One patient on a support forum wrote: “Nausea was brutal the first three months. But now it’s manageable. My neurologist says my progression is slower than average. Can’t prove it’s the riluzole-but I’d take any chance.”
Since 2017, two other drugs have joined riluzole: edaravone and tofersen. Edaravone slows functional decline in some patients. Tofersen targets a rare genetic form of ALS (SOD1 mutations) and is given by spinal injection. Both are expensive. Both are for specific groups.
Riluzole? It’s still the baseline. The first thing every neurologist prescribes. Why? Because it works for everyone. Not perfectly. Not dramatically. But enough. And it’s been tested in thousands. Its safety profile is known. Its risks are understood.
Researchers are now testing riluzole in combination with other drugs-like sodium phenylbutyrate-to see if stacking treatments can do more than one alone. Early results are promising. The future may not be one drug, but a cocktail.
Dr. Leonard Petrucelli of the Mayo Clinic put it simply: “Riluzole will remain a cornerstone of ALS treatment for the foreseeable future.” Not because it’s perfect. But because, in a field with so few options, it’s the one we know works.
ALS research is accelerating. Gene therapies. Stem cells. New neuroprotective agents. The global ALS drug market is expected to hit $2.84 billion by 2030. But for now, riluzole remains the most prescribed drug for ALS worldwide.
It’s not a cure. It’s not even close. But for nearly 30 years, it’s been the only thing standing between patients and a faster end. That’s not nothing. That’s everything.
No. Riluzole does not cure ALS. It does not reverse damage or restore lost function. It modestly slows disease progression and extends survival by an average of 2 to 3 months. For many patients, this means extra time to complete meaningful activities with loved ones.
There’s no immediate effect. Riluzole works over months, not days. Its benefit is measured in delayed decline-not sudden improvement. Most patients don’t feel different, but neurologists track progression rates. Studies show the survival benefit becomes measurable after 6 to 12 months of consistent use.
Never stop without talking to your neurologist. Feeling worse could be the disease progressing-not a reaction to the drug. Stopping riluzole won’t speed up ALS, but it removes a small protective effect. If side effects are severe, your doctor may adjust your dose or switch formulations, but discontinuation should be a shared decision.
No. Riluzole is processed by the liver. If you have moderate to severe liver impairment (Child-Pugh Class B or C), riluzole can build up to dangerous levels in your blood. It’s contraindicated in these cases. Before starting, your doctor will check your liver enzymes and monitor them monthly for the first three months.
Yes, but they’re not replacements. Edaravone (Radicava) slows functional decline in a subset of patients and is given as an IV infusion. Tofersen (Qalsody) targets a rare genetic form of ALS (SOD1 mutations) and requires spinal injections. Neither replaces riluzole’s broad benefit. Most patients take riluzole alongside these if eligible. Riluzole remains the only drug approved for all forms of ALS.
Because it’s the only drug proven to extend survival across all ALS subtypes. Newer drugs target specific populations or symptoms. Riluzole is broad, well-studied, and affordable compared to newer options. It’s the foundation. Even with new therapies, doctors start with riluzole because it’s the one thing that has consistently, reliably given patients a few extra months.
Alec Stewart Stewart
4 02 26 / 07:32 AMI just lost my dad to ALS last year. Riluzole didn’t bring him back, but it gave us 7 extra months to watch old movies together and say all the things we never said. 🙏
Samuel Bradway
5 02 26 / 19:48 PMMy neuro told me to take it, so I did. Nausea was hell the first month, but I stuck with it. Now I’m 18 months in and still walking. Not a miracle, but it’s something.
Prajwal Manjunath Shanthappa
6 02 26 / 04:41 AMRiluzole? A 235.23 g/mol benzothiazole derivative with dubious pharmacokinetics and a 35% relative risk reduction that translates to a mere 90-day survival gain-hardly a triumph of translational medicine. The glutamate hypothesis is fundamentally flawed, and yet it persists as dogma. Truly, the pharmaceutical industry’s triumph of statistical noise over biological truth.
Wendy Lamb
7 02 26 / 01:32 AMIt’s not about curing. It’s about time.
Antwonette Robinson
8 02 26 / 01:32 AMOh wow, so riluzole gives you 3 months? That’s like buying an extra week of Netflix. Meanwhile, the drug costs $1k/month. Someone’s making bank while people cry over birthday candles. 🤑
Ed Mackey
8 02 26 / 21:04 PMi took riluzole for 14 months. liver enzymes went up, so i had to stop. felt like a failure. my doc said it’s not my fault. still wish i could’ve kept going. 💔
caroline hernandez
10 02 26 / 10:43 AMThe pharmacodynamics of riluzole are foundational in ALS management-its glutamatergic modulation via voltage-gated sodium channel inhibition and presynaptic glutamate release suppression provides neuroprotection in the excitotoxic cascade. While not curative, its role as a first-line agent is evidence-based and clinically indispensable. Adherence remains suboptimal due to tolerability, but formulation innovations like Exservan improve bioavailability and reduce GI burden. This is precision neurology in its earliest, most vital form.
Sherman Lee
12 02 26 / 02:41 AMRiluzole? Nah. I’ve read the trials. The FDA approved it because they had nothing else. Big Pharma knew it was weak but pushed it anyway. And the liver damage? That’s not a side effect-it’s a slow poison. I bet they’re hiding data on long-term neurotoxicity. And why is the thin film version so expensive? Because they’re milking the dying. 🤡
Lorena Druetta
13 02 26 / 21:50 PMTo every individual facing ALS: your courage is extraordinary. Riluzole may not reverse what has been lost, but it honors the dignity of every moment you choose to fight-for your family, for your legacy, for the quiet strength that refuses to surrender. You are not alone.